
What are AI SOAP Notes? Pros, Cons, Tools & Best Practices

Key Takeaways
- AI SOAP notes turn spoken conversation into the classic Subjective • Objective • Assessment • Plan format automatically, no more nightly chart‑catch‑up.
- Clinicians who adopt them report saving 6–10 minutes per visit and feeling noticeably less burnt out.
- Setup is usually as simple as signing in, connecting your EHR, and letting the AI listen while you work.
- The tech isn’t magic; you’ll still review and sign every note, but it does 90 % of the heavy lifting.
- Choosing the right tool comes down to specialty fit, EHR integration, pricing, and data‑security pedigree.
What Are AI SOAP Notes?
AI SOAP notes are automatically generated Subjective–Objective–Assessment–Plan summaries produced from a patient encounter by machine‑learning models that capture, transcribe, and structure clinical information in real time. By turning raw conversation into a standardized medical note within seconds, they free clinicians from manual typing and allow more face‑to‑face interaction with patients. The rest of the section can continue with benefits, typical use cases, and why the SOAP framework remains the gold standard for behavioral‑health documentation.
Section | Content |
|---|---|
Subjective | What the patient/client says about their symptoms, lifestyle, mood, etc |
Objective | Vital signs, test results, your observed findings (e.g., affect, ROM) |
Assessment | Your clinical reasoning and diagnoses. |
Plan | Next steps—meds, therapy goals, follow‑up, referrals. |
How AI SOAP Notes Work
- AI securely captures the encounter via microphone, telehealth stream, or ambient device.
- Speech is transcribed and contextual data collected – large‑vocabulary models turn audio into text while extracting vitals, meds, and key phrases.
- The engine drafts a structured SOAP note – NLP organizes subjective complaints, objective findings, assessment, and plan into the correct format.
- Clinician reviews and edits – the draft appears instantly for quick validation, edits, or EHR export, keeping final clinical judgment in the provider’s hands.
How Is an AI SOAP Note Different From Dictation?
Dictation still requires you to say the whole note or type corrections afterward. AI SOAP tools listen passively, summarize automatically, and learn your phrasing over time. It’s the difference between doing laundry yourself and having it picked up, washed, folded, and returned.
Dimension | Traditional SOAP notes | AI SOAP notes |
|---|---|---|
Creation method | Manual typing or dictation | Speech-to-text + LLM summarization |
Average time per note | 7–10 min (primary care); up to 15 min (therapy) | 1–2 min post-visit review |
Accuracy & consistency | Depends on individual; error-prone when fatigued | Model-level consistency; ±3-5 pp error range in current studies |
Integration with EHR | Often copy-paste | API or FHIR push |
Impact on burnout | Neutral or negative | Burnout decreased from 51.9% to 38.8% after 30 days |
*last verified January 2026
Best AI SOAP Note Generators
Shopping for a digital side‑kick? Here’s a lightning‑round look at the top AI scribe platforms and why they might be a perfect fit for your workflow.
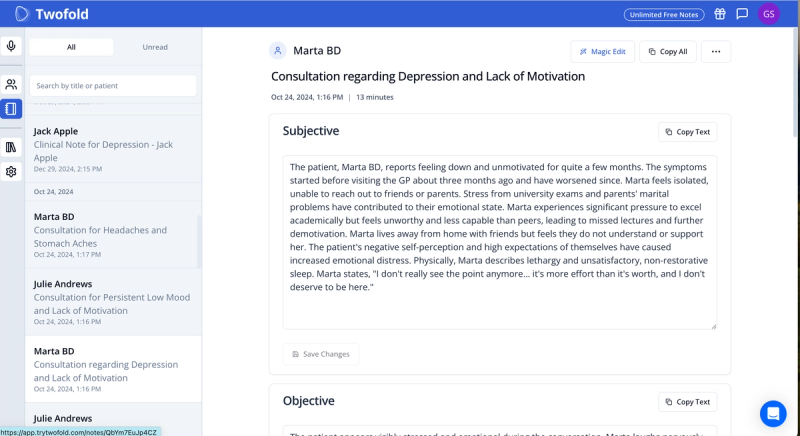
1. Twofold Health
Twofold is a real‑time AI medical scribe that adapts to each clinician’s style, making documentation faster and more accurate. It integrates seamlessly with EHR systems, ensuring a high level of accuracy, security, and customization.
Key Features
- 99% transcription accuracy with minimal need for manual correction
- AI-driven CPT/ICD-10 coding suggestions
- Specialty-based note templates
- Option to create your own templates
- Automated patient progress tracking capabilities
- Multi-language support: 25+ languages, including English, French, and Spanish
- HIPAA-compliant with enterprise-grade security
- Built-in analytics and reporting features
Pricing
- Free plan with 20 notes/month.
- $49/month unlimited access and usage.
- Group plans with volume discounts and premium offerings.
2. Athelas Scribe
Athelas Scribe is a real-time transcription tool built to handle multi‑speaker environments, various accents, and background noise. It includes automated medical coding recommendations, making it a good fit for high‑volume practices.
Key Features
- 99.4% transcription accuracy
- Multi-speaker recognition for extended conversations
- Generates SOAP notes, progress notes, and medical forms
- AI-driven CPT/ICD-10 coding suggestions
- HIPAA, SOC2, and HITRUST compliant
- Customizable formatting and templates
Pricing
- Free plan with 10 scribes
- Paid plans start at $149 per month

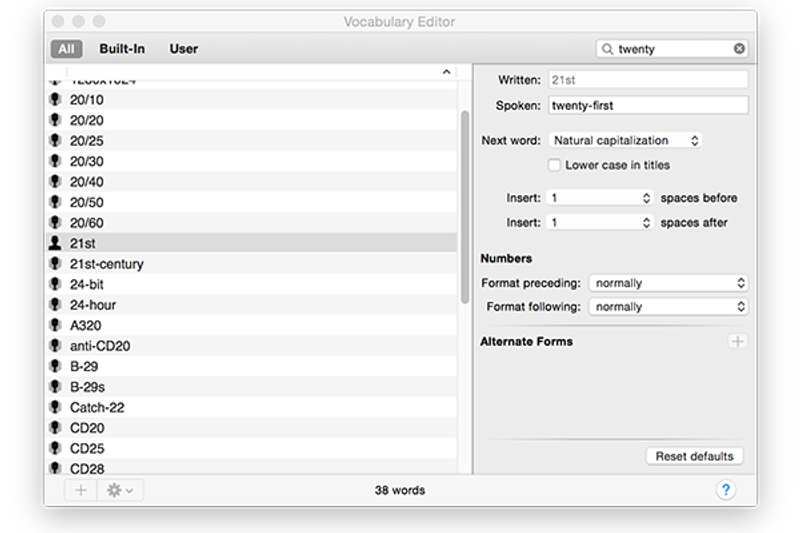
3. Nuance Dragon Medical One
Highlights:
- Leading-edge speech recognition.
- Specialized medical vocabulary.
- Enterprise-level data security.
Standout Features:
- Real-time, accurate transcription.
- Customizable medical terminology library.
- Deep integrations with enterprise EHRs.
Ideal for: Hospitals and larger healthcare organizations.
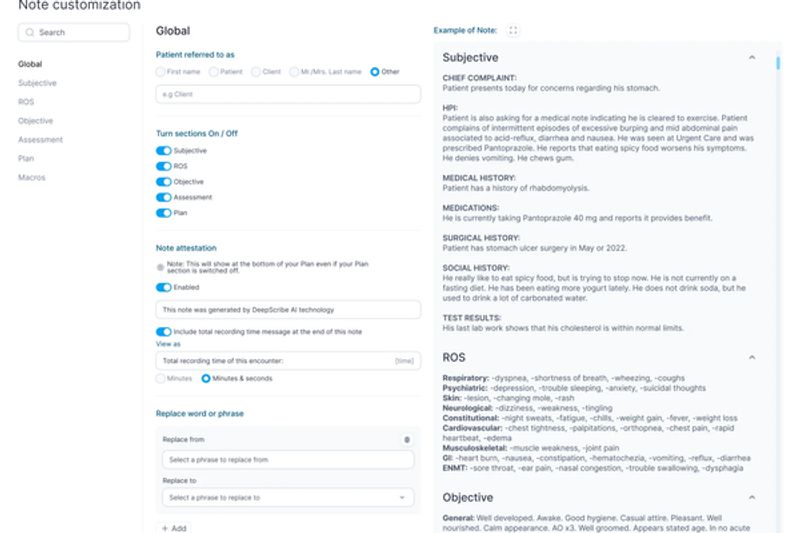
4. DeepScribe
Benefits:
- Captures conversational context effortlessly.
- Automatically summarizes and updates patient records.
- Reduces clinician burnout significantly.
Top Features:
- Conversational voice-to-text technology.
- Minimal post-editing required.
- Ideal for primary care documentation.
Benefits of AI-Generated SOAP Notes in Healthcare
1. Automated Note Generation
Sophisticated LLMs listen during the visit, classify speech by speaker and relevance, and output a complete note—including vital signs, present illness narrative, and measurable and observable data—within seconds.
2. Integration With Electronic Health Records (EHRs)
Smart APIs push both subjective and objective findings directly into discrete EHR fields, reducing redundant clicks and ensuring each SOAP note is placed where billing and quality workflows expect it.
3. Customization & Learning Capabilities
Modern systems adapt to specialty‑specific terminology (e.g., GAD‑7 or PHQ‑9 scores for mental health professionals) and learn an individual provider’s templating preferences.
4. Improved Accuracy & Consistency
A 2025 JMIR study found AI SOAP notes' quality was good to excellent overall.
5. Reduced Burnout & Increased Efficiency
A Penn Medicine study revealed that Clinicians experienced a 30% decrease in "pajama time," or after‑hours work at home, gaining about 15 minutes of personal time daily using AI scribe for note‑taking.
6. Enhanced Collaboration & Communication
Because AI SOAP notes are consistent, interdisciplinary teams can quickly scan the note, extract subjective and objective information, and act—improving hand‑offs and reducing communication errors.
Real‑world stat: In early user surveys, Twofold clinicians cut documentation time 35 % in the first month.
Challenges with Manual SOAP Note Taking
- Time‑consuming documentation – typing or dictating notes after every session steals hours each week that could be spent on patient care or revenue‑producing appointments.
- Human errors and omissions – fatigue or multitasking leads to missing vitals, misordered medications, or inconsistent assessment language that can compromise continuity of care.
- Workflow disruptions – toggling between EHR screens, note templates, and intake forms breaks clinician focus and may lengthen visit times.
- Difficulty meeting compliance standards – changing payer or state requirements makes it easy to overlook mandated elements without automated prompts.
- Delayed billing cycles – incomplete or late notes stall coding and claims submission, slowing cash flow for solo and small practices.
How to Get Started With AI SOAP Notes
Integration With Existing Systems
- Assess your EHR’s FHIR/HL7 capabilities.
- Choose “overlay” versus “in-EHR” approaches. Overlay tools such as Twofold AI Scribe run in any browser or mobile, while embedded modules require vendor marketplaces.
- Map discrete data fields such as vital signs to the EHR to unlock downstream analytics.
Training & Onboarding for Clinicians
- Kick off with a 30-minute live demo.
- Provide role-based tip-sheets that highlight where the AI populates subjective and objective findings.
- Encourage a two-week shadow phase where clinicians compare AI outputs to their existing SOAP notes.
Continuous Monitoring & Feedback
- Establish dashboards for note completeness and editing time.
- Collect clinician feedback weekly during the first month.
- Tune prompts/models when accuracy falls below 95 % or physicians spend >3 min per note.
Key Components of AI SOAP-Note Solutions
Join us as we take a closer look:
- Advanced Language Understanding with AI
Transformer-based models segment dialogue and classify it into SOAP sections in real time. - Tailored Solutions for Different Medical Fields
Mental health professionals need nuanced subjective data (affect, mood); orthopedists need physical examination findings like ROM metrics. - Instant Data Analysis and Processing
Embedded analytics flag gaps (e.g., missing present illness chronology) and recommend codes automatically. - Compliance With HIPAA and Industry Standards
Encryption in transit & at rest, Business Associate Agreements (BAAs), and audit logging are table stakes.
Pros & Cons of Using AI SOAP Notes
Let’s call it like it is: no silver bullets, just solid wins and a few trade‑offs.
Pros | Cons | |
|---|---|---|
Time efficiency | Saves 6–8 min per visit on average | Initial setup costs: Year-one ROI depends on visit volume |
Enhanced accuracy | Captures more measurable and observable data than manual typing | Learning curve: Providers need ~2 weeks to trust the output |
Consistency | Aligns documentation with payer guidelines, improving medical documentation quality | Potential technical issues: Downtime or transcription errors require fallback workflows |
Best Practices for Implementing AI SOAP Notes
Ensuring Data Security & Patient Privacy
- Host on HITRUST-certified clouds.
- Use patient consent banners when ambient listening.
- Rotate encryption keys quarterly.
Regular Training & Updates for Staff
- Quarterly in-service covering new ICD-10 mappings.
- Monthly tip-sheet on optimizing subjective and objective information capture.
Continuous Evaluation & Quality Improvement
Monitor KPIs: note completion lag, progress notes accuracy, average clicks saved, and burnout survey scores.
AI SOAP Notes Use Cases in Healthcare
Curious where this tech really shines? Peek at these day‑to‑day success stories.
Specialty | Example Use Case | AI Outcome |
|---|---|---|
Primary Care | Annual wellness visit | Auto-populated preventive-care reminders |
Mental Health | 50-min psychotherapy session | Captures nuanced mood descriptors & recommends DSM-5 codes |
Orthopedics | Post-op follow-up | Inserts operative approach, implant details, and physical exam findings |
Telehealth | Multi-state urgent care | Generates compliant interstate SOAP notes with correct time-zone stamps |
Value-Based Care | Chronic disease management | Flags missing vital signs - e.g., BP, BMI - and pushes them to quality dashboards |
AI SOAP Notes Compliance & Security
Quick reality check: compliance might feel boring, but it’s your ticket to stress‑free charting.
- HIPAA & HITECH: Ensure end-to-end encryption and signed BAA.
- GDPR (for global clinics): Offer data-processing agreements and right-to-erasure workflows.
- Audit Trails: Every edit to the SOAP note must be version-controlled.
- Model Governance: Retain prompt & response logs for 6 years, mirroring other medical documentation retention rules.
How Twofold Supercharges AI SOAP-Note Generation
Sneak peek: here’s how we turn raw conversation into crystal‑clear clinical notes in seconds.
- Smart ICD-10 “Recapture” & HCC Nudges Twofold spots chronic conditions that didn’t get coded (think COPD, diabetes) and floats a one-click suggestion before you sign—no more missed risk-adjustment revenue.
- True Plug-and-Play Onboarding Spin up your account, drop the browser extension, and you’re charting in under 10 minutes—no IT ticket, no waiting for an EHR marketplace listing. Check out our out-of-the-box SOAP note template.
- Every-EHR Overlay Our overlay grabs subjective and objective snippets even inside the most locked-down EHR screens, so you keep your workflow while we handle the paperwork.
- Adaptive Language Learning The model remembers your style (“Pt denies CP”) and mirrors it next visit, tightening consistency across progress notes and cutting edits to a minimum.
Example of a SOAP Note Created with Twofold’s AI
Patient J.D. (John Doe) MRN 3945221 DOB 1991‑07‑14
Date/Time 2025‑07‑20 14:05‑14:55 EDT Provider Emily Carter, PA‑C
Visit Type Established patient, 50‑min psychotherapy (CPT 90834)
S – Subjective
- CC: “Still anxious at work, can’t sleep through the night.”
- HPI: Workplace anxiety × 4 mo; daily worry 8/10; two brief panic episodes this month; sleep 5–6 hr with frequent awakenings.
- ROS (pertinent): +Anxiety, +Insomnia; –Depression, –SI/HI, –Chest pain.
- Meds: Sertraline 50 mg daily; Lorazepam 0.5 mg PRN (twice last 30 days); Melatonin 5 mg nightly.
- Social: Software engineer; lives with spouse; exercises 1–2×/wk; minimal alcohol; no tobacco/drugs.
O – Objective
- Vitals: BP 122/78, HR 78, RR 16, Temp 98.4 °F, SpO₂ 99 % (room air).
- MSE: Well‑groomed, cooperative, normal speech, mood “anxious but hopeful,” congruent affect, logical thought, no delusions or SI/HI, A&O × 4, good insight/judgment.
A – Assessment
- Generalized Anxiety Disorder (F41.1) – partially controlled; ongoing insomnia and situational stress. No depressive episode or acute safety concerns.
P – Plan
- Medication: Increase Sertraline to 75 mg PO daily; continue Lorazepam 0.5 mg PRN ≤3×/wk.
- Therapy: Continue weekly CBT; next focus on perfectionism reframing; add guided breathing app nightly.
- Lifestyle: Consistent lights‑out 23:00; screen‑free 30 min before bed; evening walks 3×/wk.
- Follow‑up: Virtual visit in 4 weeks; complete PHQ‑9 & GAD‑7 via portal beforehand; sooner if adverse effects or symptom escalation.
- Education/Consent: Discussed med risks/benefits; patient verbalized understanding and agreement; provided CBT journaling handout.
Conclusion
AI SOAP notes aren’t just a trendy gadget; they’re a practical way to claw back hours, create crystal‑clear documentation, and put your focus back where it belongs—on your patients. Start small, track your gains, and adjust as you go. Within a couple of weeks, you’ll wonder how you ever lived without them.
Ready to try it risk‑free? Grab a Twofold trial and let your next patient visit write itself.

Dr. Danni Steimberg
Dr. Danni Steimberg is a pediatrician at Schneider Children’s Medical Center with extensive experience in patient care, medical education, and healthcare innovation. He earned his MD from Semmelweis University and has worked at Kaplan Medical Center and Sheba Medical Center.
- Spend the first week running Twofold side‑by‑side with your existing note‑taking method.
- Compare the AI draft to your manual notes, highlight discrepancies, and feed corrections back into the system.
- Clinicians who complete this “shadowing” phase report a 30–50 % reduction in edits once they switch fully, because the model has adapted to their terminology and preferred phrasing.
Frequently Asked Questions
ABOUT THE AUTHOR
Dr. Eli Neimark
Licensed Medical Doctor
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

From Intake To Progress Notes: How AI Handles The Whole SOAP Chain
See how AI manages the entire documentation workflow from initial patient intake, ensuring consistency.
AI Scribe FAQ: What People Are Really Asking on Reddit, Professional Forums & LLMs (2025 Edition)
Discover the real‑world questions clinicians ask about AI medical scribes - legality, HIPAA, accuracy, consent, specialty fit & more - answered by experts.

The Most Affordable AI Scribe 2026 (US Edition)
See 2026 US pricing for popular AI scribes. Twofold Health leads on affordability at $49/mo (annual) with unlimited notes, undercutting Freed, Heidi, and Scribeberry.

