
How to Write SOAP Notes: Examples & Template

What is a SOAP Note?
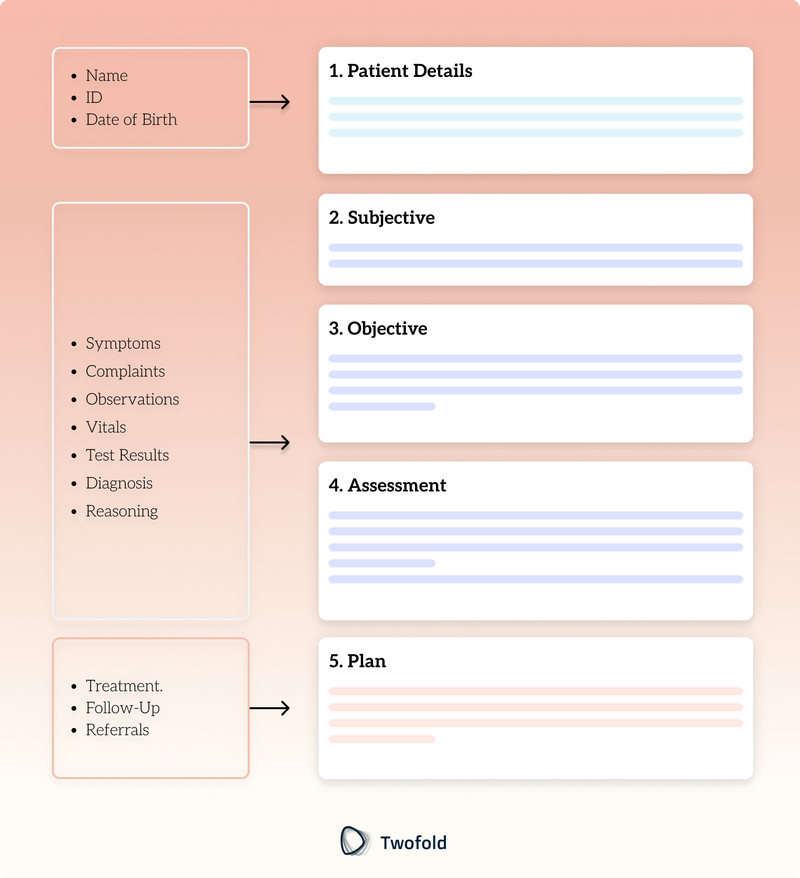
SOAP notes are a widely used method of documentation in healthcare, valued for their simplicity, structured format, and adaptability. They organize client or patient information into four key categories: Subjective, Objective, Assessment, and Plan, ensuring comprehensive and accurate record‑keeping. Here’s a closer look at each component:
Subjective (S):
Details the client’s condition and history, including major or minor complaints and whether the issue is recent or long‑term.
Objective (O):
Captures measurable and observable data gathered during the clinical encounter, both quantitatively and qualitatively.
Assessment (A):
Provides the therapist’s evaluation of the client’s condition, along with an interpretation of findings.
Plan (P):
Outlines the recommended treatment, follow‑up care, and any actions required for future correspondence.
Developed in the mid‑1960s by Dr. Lawrence Weed as part of the problem‑oriented medical record system, SOAP notes have since become an indispensable documentation approach across various fields, including medicine, nursing, physical therapy, and mental health.
How to Write SOAP Notes
SOAP notes adhere to a structured format designed to comprehensively document all aspects of a client’s visit to a therapist. Here’s a detailed guide to organizing your SOAP notes, ensuring clarity and thoroughly addressing the client’s history and current status.
Draft and Organize Your SOAP Notes
Simply start by organizing your notes into the four SOAP sections:
- Subjective: Record the client’s verbal description of their symptoms, concerns, and history. Include quotes where relevant to capture their perspective accurately.
- Objective: Document measurable and observable data, such as physical exam findings, vital signs, and test results.
- Assessment: Analyze the subjective and objective data to reach a potential diagnosis or record and update the client’s progress.
- Plan: Outline the next steps, including treatment options, follow-up appointments, or diagnostic tests.
Review and Interpret Your SOAP Notes
- Once you have completed drafting, review your notes for accuracy.
- Cross-check client's information for consistency between sections.
- Verify that the ‘Plan’ section is actionable and detailed and addresses all critical issues raised during the visit.
- Regularly reviewing SOAP notes will improve their quality and ensure they provide a complete clinical picture.
Enhance Your SOAP Notes with AI
- AI can convert client conversations into draft SOAP notes, saving time.
- It can highlight any inconsistencies or missing information for a more thorough review.
- AI can analyze patterns in client data, helping you refine your assessments and plans.
- By incorporating AI, you can reduce manual effort while maintaining high documentation standards.
Simplify and Standardize with Templates
- Templates provide ready-to-use sections for Subjective, Objective, Assessment, and Plan.
- Templates should be developed with certain practices or specialties in mind.
- Using templates ensures that providers consistently follow established protocols tailored to particular contexts.
- Templates make taking notes easier and help avoid missing important information.
SOAP Note Example for Mental Health Counseling
SOAP analysis is a valuable tool for counseling sessions, providing a structured framework to document key information clearly and comprehensively. Below is an example demonstrating how each section can be applied in a mental health counseling session:
S: Subjective
This section captures the client’s verbalized thoughts, feelings, and perceptions about their current state. It focuses on what the client shares during the session.
Example: The client stated, “I’ve been feeling overwhelmed and anxious lately. I can’t concentrate at work, and I keep worrying about things going wrong.” The client also reported having trouble sleeping, along with frequent headaches.
O: Objective
This section records the counselor’s factual observations during the session, including physical appearance, behavior, and non‑verbal cues.
Example: The client appeared restless, frequently fidgeting with their hands. Their voice was subdued, and they avoided eye contact throughout the session. No physical impairments or abnormalities were observed.
A: Assessment
In this section, the counselor evaluates the client’s mental health condition, progress, and engagement with therapy. It may include a diagnosis or a summary of the session.
Example: The client is exhibiting symptoms of Generalized Anxiety Disorder (GAD), such as excessive worry, difficulty concentrating, and physical symptoms like headaches and disrupted sleep. The client appears motivated to work on these issues and is open to therapeutic interventions.
P: Plan
This section outlines the next steps for treatment, including interventions, goals, and any changes in the therapeutic approach.
Example: The client will practice a 10-minute mindfulness meditation exercise daily to help manage anxiety. The therapist will introduce Cognitive Behavioral Therapy (CBT) techniques in the next session to address thought distortions. Follow-up is scheduled for next Tuesday.
SOAP Note Template
Benefits of Using SOAP Notes
SOAP notes offer mental healthcare professionals several advantages, including:
- Tracking Progress and Identifying Patterns: By systematically documenting each session, SOAP notes help therapists monitor a client’s progress or setbacks over time. This continuity supports the development of effective strategies and therapeutic approaches tailored to the client’s needs.
- Facilitating Information Sharing: SOAP notes standardize documentation, making it easier to share critical client information with other healthcare providers. This is especially valuable when coordinating care across multiple specializations or disciplines.
- Improved Client Care: The structured format of SOAP notes enables therapists to focus on personalized treatment plans. The progressive nature of the notes ensures that each session builds on previous ones, contributing to a more efficient and cohesive treatment process.
Common Challenges in Writing SOAP Notes
Writing an effective and completely up‑to‑date SOAP note can be challenging. This problem is particularly common in people new to the process or working in fast‑paced clinical environments.
Challenges | Description | Solution |
|---|---|---|
Decoding and Simplifying Jargon | Acronyms and technical terms can obscure the meaning of SOAP notes, making them hard for clients or other medical practitioners to understand. | Use plain language and avoid unnecessary jargon to ensure clarity and accessibility for a broad audience. |
Balancing Clarity and Detail | Providing too much detail can confuse the reader, while limited details may omit critical information. Repetition and lengthy phrases also reduce clarity. | Use concise phrasing, avoid repetition, and ensure critical information is included without overloading the note. |
Handling Time Constraints for Documentation | Time pressure in clinical settings often results in rushed or incomplete notes, potentially affecting their accuracy and usefulness. | Use templates, AI software, and pre-charting to streamline documentation and reduce time pressure. |
Differentiating Subjective Insights from Objective Data | Mixing subjective client-reported symptoms with objective clinical findings can compromise the accuracy of SOAP notes, leading to ineffective assessments. | Each section is clearly delineated, with client-reported symptoms recorded under "Subjective" and clinical observations documented in the "Objective" section. |
Best Practices for Writing Effective SOAP Notes
Crafting accurate and comprehensive SOAP notes can be difficult, especially for those new to the process or operating in high‑pressure clinical settings. Adhering to some best practices can significantly help with these challenges, ensuring clarity, consistency, and efficiency in documentation:
1. Maintaining Consistency
Consistency is key to making SOAP notes easy to follow and reliable. Follow the SOAP format ‑ Subjective, Objective, Assessment, and Plan ‑ strictly to ensure that each note is legible and that all the puzzle pieces fit where they are supposed to. Moreover, SOAP notes should be written promptly to prevent a break or mixture of client record information.
2. Avoiding Common Errors
Minimize errors in SOAP notes to prevent misinterpretations. Avoid vague statements and focus on specifics. For instance, replace "client feels better" with "client reports a 50% reduction in pain after medication administration." Pay close attention to detail when documenting signs, symptoms, investigations, and treatment plans.
Refrain from inserting personal opinions or assumptions into the notes; let the data speak for itself. Additionally, ensure that any unresolved issues, pending tests, or follow‑up actions are clearly documented to maintain continuity of care.
3. Ensuring Compliance with Regulations
SOAP notes must meet legal and regulatory standards to protect both clients and providers. Abide by HIPAA or other relevant laws to preserve the clients’ anonymity. It is advisable not to incorporate excessive identifiable information.
SOAP Note Abbreviations Explained
Here’s a breakdown of common abbreviations used in mental health counseling SOAP notes:
Section | Abbreviations |
|---|---|
Subjective |
|
Objective |
|
Assessment |
|
Plan |
|
SOAP Notes With Twofold
Twofold Health streamlines SOAP note documentation for healthcare professionals across specialties. Here’s how it improves your workflow:
Prebuilt SOAP Templates
Choose from ready‑to‑use templates designed for general healthcare and specialty practices, including streamlined formats that combine sections.
Customizable Documentation
Modify existing templates or create custom formats tailored to your field. Add, remove, or reorder sections to align with specific workflows.
AI-Powered Note Creation
Twofold’s AI generates draft SOAP notes from session data, checks for missing details, and provides actionable insights to enhance treatment planning.
Efficiency Features
Save time with pre‑filled prompts, one‑click copying, and tools for effortlessly managing multiple notes.
Secure and Compliant
All documentation complies with HIPAA and other regulatory standards, ensuring patient information remains protected.
Twofold Health offers a fast, flexible, and secure solution for SOAP notes, enabling healthcare providers to focus on delivering high‑quality care.
Conclusion
SOAP notes are crucial in healthcare settings as they provide a structured method for documenting a client’s condition. They not only enhance communication by simplifying the documentation process, but also ensure legal compliance. When healthcare professionals master the SOAP format and consistently apply its four components, it leads to higher‑quality care, improved client outcomes, and stronger collaboration among caregiving teams.
Frequently Asked Questions
ABOUT THE AUTHOR
Dr. Andleeb Asghar
Research Collaborator
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

The Best AI Scribe in 2026 - According to Real Facebook Reviews (2026)
We read real Facebook reviews to rank the best AI scribe tools of 2026. See authentic quotes, pros & cons, and find your recommended AI scribe fast.

Can An AI Scribe Keep Up With A 15-Minute Visit?
Can AI truly document a fast-paced patient visit? Explore the capabilities and limits of AI medical scribes in real-world settings.

How Much Time Can You Save With an AI Scribe?
Reclaim your evenings and reduce burnout. See how an AI scribe automates documentation, giving you hours of your week back.

