
90791 CPT Code: Guide to Initial Intake Appointment

Key Takeaways
- CPT Code 90791 is used exclusively for psychiatric diagnostic evaluations without medical services, primarily during initial intake sessions, allowing eligible licensed professionals to bill for comprehensive assessments.
- Accurate documentation and compliance with state and insurance-specific regulations are essential for properly billing CPT Code 90791 to avoid claim denials and ensure reimbursement rates are upheld.
- The 2024 reimbursement rate for CPT Code 90791 has decreased to $169.29, and the code can be billed annually for Medicare and Medicaid services, with variations in billing frequency based on specific insurance guidelines.
Understanding CPT Code 90791
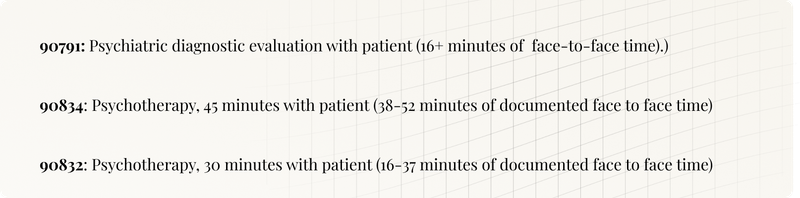
CPT Code 90791 is used for psychiatric diagnostic evaluations without involving medical services. This code is typically billed for intake appointments where a comprehensive assessment is conducted without the involvement of medical interventions. It encompasses a thorough evaluation of the patient’s history, mental status, and the formulation of treatment recommendations.
Licensed professionals eligible to bill for CPT Code 90791 include Clinical Social Workers, licensed professional counselors, Mental Counselors, Marriage and Family Therapists, licensed marriage family therapists, Clinical Psychologists, and Psychiatrists. Some states may have restrictions on who can bill for this code, impacting non‑psychiatrists.
Correct use of CPT Code 90791 ensures accurate reimbursement for the services provided. Misuse of this code can lead to claim denials and financial losses, so mental health professionals must be well‑versed in its application and billing requirements.
When to Use CPT Code 90791
CPT Code 90791 is primarily used for the initial intake session of clients with new behavioral health issues. This code covers a comprehensive biopsychosocial assessment, which evaluates the patient’s history, mental status, and provides treatment recommendations. It is especially useful for gathering background information and setting goals during intake sessions.
The typical session time for CPT Code 90791 is around 60 minutes, although it can vary from a minimum of 16 minutes to a maximum of 90 minutes. This flexibility allows mental health professionals to conduct thorough evaluations tailored to each client’s needs. Additionally, this code can be used for initial evaluations as well as yearly progress checks.
Mental health professionals should check state laws and regulations regarding the use of CPT Code 90791. States may have different guidelines on who can bill for this code and under what circumstances, so staying informed and compliant with local regulations is crucial.
Documentation Requirements for 90791
Accurate documentation is crucial when billing for CPT Code 90791. The documentation must reflect a direct interaction between the provider and the client. Valid billing requires the initial mental health evaluation to include a detailed medical and psychiatric history and a mental status examination.
Insurance providers, including Medicare, often require that the clinical notes detail the patient’s capacity to engage in treatment. This includes summarizing the client’s diagnosis, symptoms, and functional status, as well as providing complete medical documentation to establish medical necessity. Additionally, the duration of the session and the treatment modality used must be documented to meet insurance requirements.
Another crucial aspect of documentation for CPT Code 90791 is the initial treatment plan. This plan should outline the proposed interventions and goals for the client’s treatment, providing a roadmap for future sessions. Proper documentation ensures compliance with billing standards and enhances care quality by establishing clear treatment objectives.
Reimbursement Rates for CPT Code 90791 in 2024
In 2024, the reimbursement rate for CPT Code 90791 is $169.29, slightly lower than the 2023 rate of $174.86. Despite the decrease, CPT Code 90791 generally yields higher reimbursement rates compared to follow‑up session codes like 90834 and 90837.
Reimbursement rates can vary based on the provider’s credentials. Providers with licenses other than Ph.D. or MD typically receive lower reimbursement rates for CPT Code 90791.
The rates set by the Centers for Medicare Services (CMS) apply nationally, ensuring a standardized approach to reimbursement.
Frequency of Billing CPT Code 90791
Before: CPT Code 90791 can be billed once per client per provider annually for Medicare and Medicaid services, and Medicare covers this code for institutionalized patients once per year. Some private insurance plans may allow billing CPT Code 90791 once every six months. Checking each insurance plan’s specific guidelines can help avoid claim denials.
After: CPT Code 90791 can be billed:
- Once per client per provider annually for Medicare and Medicaid services
- Once per year for institutionalized patients under Medicare
- Once every six months for some private insurance plans
Checking each insurance plan’s specific guidelines can help avoid claim denials.
Billing CPT Code 90791 more frequently than allowed by the patient’s insurance can result in claim denials and delays in reimbursement. Mental health professionals must stay informed about the billing frequencies permitted by different insurance providers to ensure compliance and avoid financial setbacks.
Differences Between CPT Codes 90791 and 90792
Aspect | CPT Code 90791 | CPT Code 90792 |
|---|---|---|
Focus | Psychiatric evaluations without medical interventions | Psychiatric evaluations including medical services |
Usage | Comprehensive evaluations | Includes medical services (e.g., prescriptions, physical exams) |
Eligible Providers | Licensed mental health providers (e.g., social workers, licensed mental health counselors) | Licensed clinical social workers and other licensed behavioral health providers |
Medical Activities | Not applicable | Writing prescriptions, performing physical exams, modifying treatment |
Suitability | Suitable for evaluations without medical needs | Suitable for patients requiring medical interventions in addition to evaluations |
Add-On CPT Codes for Extended Sessions
For sessions exceeding 90 minutes using CPT Code 90791, recommended add‑on codes should be used. These add‑on codes ensure providers are adequately compensated for extended time spent on evaluations.
Mental health professionals should use these add‑on codes during integrated biopsychosocial assessment, where detailed patient information is gathered. If unsure about the appropriate add‑on codes, consulting a mental health billing service can be beneficial.
Authorization Requirements for CPT Code 90791
Authorization is usually not necessary for billing CPT Code 90791, although certain insurance plans may require it. Some insurance providers may only provide one authorization for CPT Code 90791 before requiring another code for subsequent sessions.
Often, only a single authorization is granted for CPT Code 90791, after which other codes must be used. Mental health professionals should be aware of these limitations to ensure compliance with insurance requirements and avoid disruptions in patient care.
Common Errors in Billing 90791
Common errors in billing CPT Code 90791 include incorrect usage of CPT codes, leading to delays in reimbursement and claim denials. Proper knowledge if medical billing can minimize these errors, resulting in quicker reimbursements and less administrative burden for mental health professionals.
Benefits of Insourcing Medical Billing
By keeping medical billing in‑house, mental health services practitioners can maintain direct control over billing processes, ensuring they align closely with the practice's specific needs and standards. This approach allows providers to develop a deeper understanding of their billing practices, which can enhance their ability to address new behavioral health concerns effectively and deliver high‑quality care.
Insourcing helps mental health providers build internal expertise in medical billing practices, reducing reliance on external services. With a dedicated in‑house billing team, practitioners can navigate complex insurance requirements more effectively, improving claim processing efficiency and ensuring timely reimbursements.
Maintaining medical billing internally can aid practitioners in ensuring accuracy and compliance in coding for CPT Code 90791. This approach ensures that all services provided are precisely documented and billed, reducing the risk of claim denials and financial losses.
Importance of Accurate Coding for 90791
Accurate coding for CPT Code 90791 ensures correct reimbursement and compliance with insurance regulations. Healthcare providers skilled in accurate coding can manage their practices effectively and minimize claim denials.
Understanding coding guidelines for 90791 helps mental health professionals streamline their billing processes. This knowledge allows for precise documentation and efficient billing practices, contributing to the practice’s overall success.
Specialized billing experts and AI‑driven coding tools can improve compliance with coding guidelines and reduce billing errors. These tools often include features like CPT/ICD code searches and detailed reporting capabilities, making the coding process more manageable and accurate.
Tools and Services to Assist with Billing
Various tools are available to help get the documentation right for CPT Code 90791. AI‑generated programs like Twofold AI Scribe can streamline the documentation process, making it easier for mental health professionals to meet billing requirements.
Integrating AI software with existing EHR systems can further streamline billing. Automated coding solutions can significantly reduce the time spent on manual coding tasks, allowing mental health professionals to focus more on patient care.
Summary
Understanding and correctly utilizing CPT Code 90791 is crucial for mental health professionals who want to ensure accurate billing and optimal reimbursement. From knowing when to use the code and meeting documentation requirements to understanding reimbursement rates and avoiding common billing errors, each aspect plays a vital role in the financial health of a practice.
By leveraging tools and services to assist with billing and considering the benefits of outsourcing, mental health providers can focus more on patient care and less on administrative tasks. Accurate coding is not just about compliance; it’s about providing the best possible care to patients by ensuring that all services are properly documented and reimbursed.
Enhance your practice with an AI medical scribe to streamline documentation and improve patient care.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

F43.12 ICD-10 Code: PTSD, Chronic
Discover essential insights on the F43.12 ICD-10 Code code for health professionals. Enhance your practice and navigate billing with confidence.

90875 CPT Code: Psychophysiological Therapy with Biofeedback
Discover essential insights on the 90875 Psychophysiological Therapy with Biofeedback, 30 minutes CPT code for health professionals. Enhance your practice and navigate billing with confidence.

F41.9 ICD-10 Code: Anxiety Disorder, Unspecified
Discover essential insights on the F41.9 ICD-10 Code code for health professionals. Enhance your practice and navigate billing with confidence.

