
Behavioral Health Progress Note Template
So you're sitting there with a cup of coffee, basking in the tranquility of the morning light, when it dawns on you that it’s time to fine‑tune your documentation process for behavioral health progress notes. You remember those moments of frustration when critical details were missed, leading to inaccurate records and potential delays in patient care. You're in luck because we are diving into the Behavioral Health Progress Note Template, your new best friend in documentation.
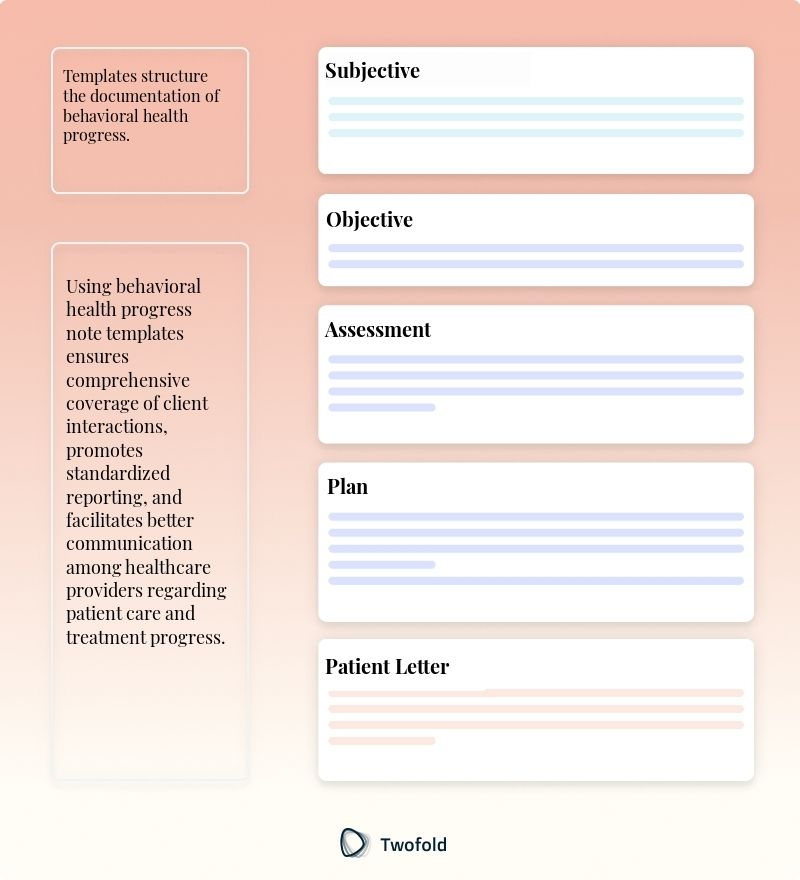
What Is a Behavioral Health Progress Note Template?
A Behavioral Health Progress Note Template is a framework designed to document patient interactions and therapeutic sessions effectively and efficiently. It serves as a guide to ensure that all relevant information is captured systematically during each patient encounter.
This type of template ensures consistent documentation across different providers and sessions, making it an essential tool for delivering high‑quality care and maintaining accurate medical records.
Key Components of a Behavioral Health Progress Note
This template integrates various elements needed for comprehensive note‑taking. Key components include:
- Patient Identification Information
- Session Date and Duration
- Patient's Presenting Problem
- Current Mental Status
- Treatment Goals and Objectives
- Treatment Interventions Used
- Patient's Progress Towards Goals
- Plan for Future Treatment
- Provider's Signature and Credentials
How to Use a Behavioral Health Progress Note Template: Step-by-Step Process
- Begin by entering basic patient identification details like name and age.
- Document the date and time of the session, along with its duration.
- Describe the patient's presenting problem, highlighting any changes since the last session.
- Record key observations about the patient's current mental status.
- Outline the specific treatment goals and objectives discussed during the session.
- Detail the interventions applied during the session and the patient's response.
- Comment on the patient's progress in achieving the outlined goals.
- Plan and document future treatment steps and any adjustments needed.
- Conclude by signing the note with your credentials for professionalism and accountability.
Benefits of a Behavioral Health Progress Note
Benefit | Description |
|---|---|
Enhanced Clarity | Provides a structured approach to note-taking that minimizes ambiguity. |
Improved Efficiency | Streamlines documentation processes, saving time for healthcare providers. |
Consistent Record-Keeping | Ensures that documentation is uniform across different sessions and providers. |
Better Patient Care | Facilitates comprehensive tracking of patient progress and treatment effectiveness. |
Stakeholders in Behavioral Health Progress Note
Several key parties have a vested interest in the effective use of these templates:
- Behavioral Health Professionals: Psychiatrists and psychologists access these templates to track patient progress accurately, making informed decisions on treatment adjustments.
- Healthcare Administrators: Utilize this comprehensive documentation to streamline workflow and enhance patient management systems.
- Insurance Providers: Depend on detailed notes to verify treatment claims and ensure compliance with health regulations.
- Patients: Benefit from the transparent recording of their treatment journey, allowing for better self-awareness and active participation in their care.
Example of a Behavioral Health Progress Note
Below is a quick walkthrough of how a behavioral health progress note can be structured effectively:
Real-World Use Cases: Practical Impact of the Behavioral Health Progress Note Template
These templates play an integral role in various scenarios, proving their versatility and impact.
- Busy clinic: In a bustling clinic, a psychologist uses these notes to quickly and effectively communicate a patient's progression through cognitive behavioral therapy to a new attending therapist, ensuring continuity of care.
- Insurance: Insurance companies frequently rely on detailed notes to corroborate the necessity of ongoing treatment, granting pre-approval for additional sessions.
- Family sessions: During family consultations, professionals use these templates to document discussions, aligning treatment goals with family expectations and ensuring that everyone is on the same page.
Conclusion
In summary, the Behavioral Health Progress Note Template is a crucial tool in ensuring consistent, efficient, and clear documentation of patient interactions. By leveraging this template, healthcare professionals can improve patient care, streamline administrative tasks, and foster collaborative environments amongst clinicians. Adopt and adapt this template to meet the dynamic needs of your practice, ensuring precise and personalized patient care.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.

Dr. Danni Steimberg
Dr. Danni Steimberg is a pediatrician at Schneider Children’s Medical Center with extensive experience in patient care, medical education, and healthcare innovation. He earned his MD from Semmelweis University and has worked at Kaplan Medical Center and Sheba Medical Center.
Documenting subtle shifts in behavior and mindset is critical—especially in therapy settings. Refined through real‑world sessions, this tactic ensures each note stands out for clinical clarity and reimbursement.
- Pinpoint Small Wins: Note incremental changes in mood or coping skills, reinforcing progress for the client and justifying continued therapy (e.g., CPT 90837).
- Record Specific Interventions: Reference your clinical methods (CBT, motivational interviewing) in each note to tie outcomes directly to techniques used.
- Plan the Next Step: End every note with a roadmap—whether adjusting interventions or scheduling more frequent sessions—to highlight ongoing medical necessity.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

Patient Demographics Template
Discover practical Patient Demographics templates to enhance your documentation efficiency.

Needs Assessment Template
Discover practical Needs Assessment templates to enhance your documentation efficiency.

Treatment Summary Template
Discover practical Treatment Summary templates to enhance your documentation efficiency.


