
Psychiatric Soap Note Template
Imagine you're sitting at your desk, scrolling through a heap of paperwork that never seems to dwindle. You're a mental health professional looking for better ways to streamline documentation without compromising on patient care. You've stumbled upon the idea of Psychiatric SOAP Notes but are unsure of how to effectively harness their benefits. You're in the right place to gain insights into making this documentation tool work for you.
What Is a Psychiatric Soap Note Template?
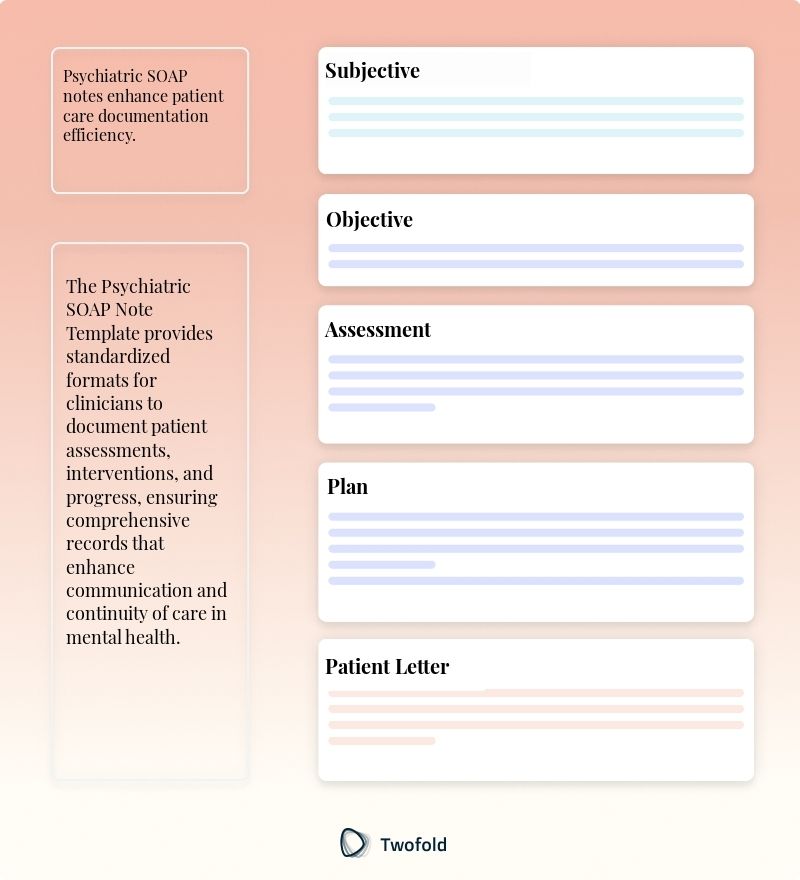
The Psychiatric SOAP Note Template is a structured format used by mental health practitioners to document patient sessions. SOAP is an acronym for Subjective, Objective, Assessment, and Plan, representing the four major components of the note.
This template helps provide a comprehensive view of a patient’s mental health status and treatment plan. It ensures consistent documentation practices, allowing for clear communication among healthcare providers and better patient outcomes.
Key Components of a Psychiatric SOAP Note?
A well‑structured psychiatric SOAP note consists of several essential parts:
- Subjective: Includes the patient’s verbal expressions about their feelings and symptoms.
- Objective: Observations made by the clinician, including appearance, behavior, and vital signs.
- Assessment: Clinician’s evaluation and diagnosis based on the subjective and objective data.
- Plan: Describes the proposed treatment strategy and any necessary follow-ups.
How to Use a Psychiatric SOAP Note Template: Step-by-Step Process
- Begin with patient identification details for accurate recordkeeping.
- Under "Subjective," note patient-reported symptoms and concerns.
- In the "Objective" section, include observable data such as mood or appearance.
- Write the "Assessment," detailing your clinical interpretation and diagnosis.
- Conclude with the "Plan," specifying treatment options and next steps.
Benefits of a Psychiatric SOAP Note
Benefit | Description |
|---|---|
Enhanced Communication | Ensures all team members have access to detailed patient progress and care plans. |
Time Efficiency | Reduces time spent on documentation, allowing more focus on patient care. |
Standardization | Promotes consistency and clarity in patient records across different providers. |
Stakeholders in Psychiatric SOAP Note
Several stakeholders interact with or benefit from well‑constructed psychiatric SOAP notes:
- Mental Health Practitioners: Use the template for accurate patient progress tracking. Dr. Smith updates his notes after each session to ensure continuity of care.
- Patients: Benefit from clear and structured documentation of their treatment progress, as seen when Maria reviews her care plan before a follow-up session.
- Healthcare Teams: Leverage the notes for interdisciplinary collaboration. Nurses and therapists at Hope Clinic share insights during weekly meetings.
Example of a Psychiatric SOAP Note
A well‑structured example can illustrate a patient session with essential details maintained while ensuring adherence to the SOAP format.
Real-World Use Cases: Practical Impact of the Psychiatric SOAP Note Template
Pyschiatric SOAP notes have transformative impacts across various healthcare scenarios:
- In a bustling urban clinic, Dr. Patel finds the standardized template essential for managing a high volume of patients while providing individualized care.
- A rural mental health center uses these notes to maintain continuity of care as patients transition between providers due to staffing changes.
- During a community health crisis, therapists efficiently adjusted treatment plans by quickly reviewing past SOAP notes, ensuring responsive care.
Conclusion
The Psychiatric SOAP Note Template is an invaluable tool for streamlining documentation, fostering clear communication, and ensuring effective mental health care. By understanding the key components and deriving benefits from this structured approach, mental health professionals can enhance patient outcomes and work more efficiently.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.

Dr. Danni Steimberg
Dr. Danni Steimberg is a pediatrician at Schneider Children’s Medical Center with extensive experience in patient care, medical education, and healthcare innovation. He earned his MD from Semmelweis University and has worked at Kaplan Medical Center and Sheba Medical Center.
Psychiatric SOAP notes require both clinical precision and nuanced insight. This tried‑and‑true method ensures your notes remain thorough, accurate, and actionable.
- Subjective: Capture Key Symptom Narratives
Encourage the patient’s own words on mood shifts, sleep patterns, or thought changes—this personal perspective is essential for treatment refinement. - Objective: Document Observable Behaviors
Include mental status exam findings, vital signs, and any physical indicators to ground your notes in measurable data. - Assessment: Tie Findings to Diagnosis
Link subjective and objective data to refine or confirm diagnoses (e.g., Major Depressive Disorder), justifying your chosen codes. - Plan: Outline Treatment & Next Steps
Specify changes in medication or therapy strategies, ensuring each intervention directly follows from your assessment.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

Case Conceptualization Template
Discover practical Case Conceptualization templates to enhance your documentation efficiency.

Family Therapy Note Template
Discover practical Family Therapy Note templates to enhance your documentation efficiency.

Symptom Tracker Template
Discover practical Symptom Tracker templates to enhance your documentation efficiency.


