
Psychotherapy Progress Note Template
Key Takeaways
- A psychotherapy progress note streamlines the documentation process for mental health professionals.
- It ensures consistency and accuracy in recording client progress and therapeutic interventions.
- Templates can be customized to fit individual or group therapy sessions.
What Is a Psychotherapy Progress Note?
A psychotherapy progress note is a vital tool used by mental health practitioners to document the details of therapy sessions. These notes capture essential information about the client's progress, the therapeutic interventions used, and any changes in the treatment plan.
Unlike psychotherapy notes, which are more personal reflections of the therapist, progress notes serve as legal documents that can be shared with other healthcare providers and insurance companies. They are crucial for maintaining a clear record of the client's treatment journey.
Key Components of a Psychotherapy Progress Note
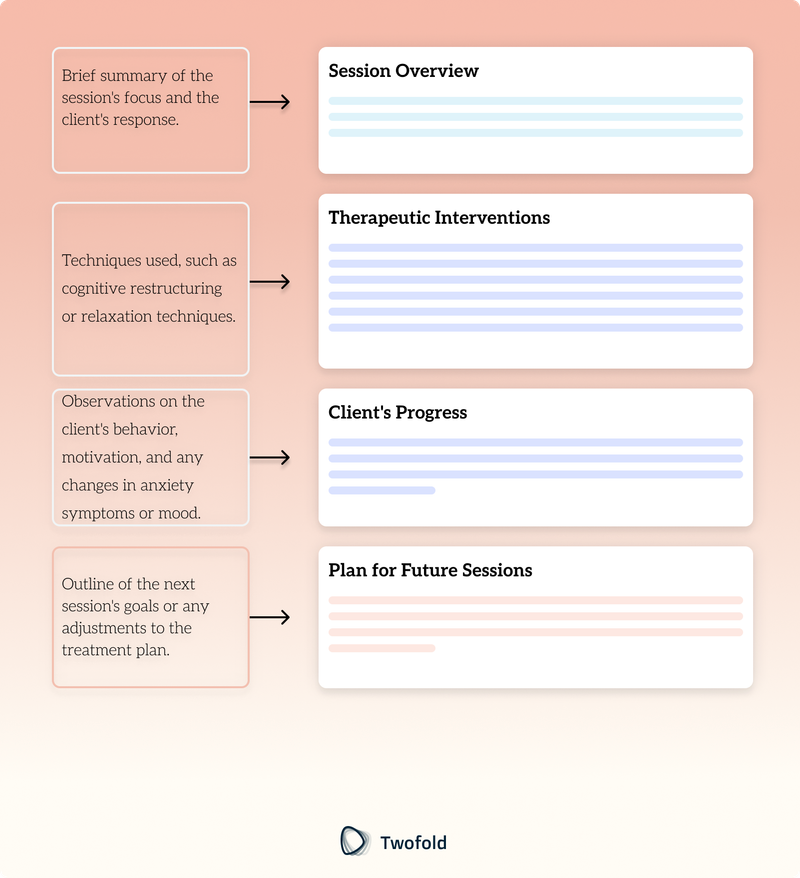
A well‑structured psychotherapy progress note typically includes:
- Client Information: Name, date of birth, and session date.
- Session Overview: Brief summary of the session's focus and the client's response.
- Therapeutic Interventions: Techniques used, such as cognitive restructuring or relaxation techniques.
- Client's Progress: Observations on the client's behavior, motivation, and any changes in anxiety symptoms or mood.
- Plan for Future Sessions: Outline of the next session's goals or any adjustments to the treatment plan.
How to Use a Psychotherapy Progress Note: Step-by-Step Process
Step 1: Gather Client Information
Begin by entering the client's details, including their name, date of birth, and the date of the therapy session. Having accurate client information is crucial for maintaining organized records and ensuring that each session is correctly attributed to the right individual. This step also helps in tracking the client's therapy journey over time and can be beneficial when collaborating with other mental health professionals or healthcare providers.
Step 2: Summarize the Session
Provide a brief overview of the session, highlighting key points discussed and the client's response to therapeutic interventions. This summary should capture the essence of the session, noting any significant breakthroughs or challenges faced by the client. Including the client's emotional state and any notable changes in their demeanor can offer valuable insights for future sessions. Additionally, this section serves as a quick reference for therapists to recall past sessions and plan subsequent ones effectively.
Step 3: Document Therapeutic Interventions
Detail the specific techniques used during the session, such as identifying triggers or using supportive counseling. It's important to note how these interventions were received by the client and any immediate effects observed. This documentation not only aids in evaluating the effectiveness of different techniques but also supports the therapist in refining their approach to better suit the client's needs. Recording the interventions also ensures that the therapy aligns with the client's treatment plan and goals.
Step 4: Assess Client's Progress
Note any significant changes in the client's behavior, mood, or motivation, and document any risk assessments conducted. This assessment should include both subjective observations and objective data, providing a comprehensive view of the client’s progress. Understanding the client's development or any setbacks can guide adjustments in therapeutic strategies and foster a more personalized treatment approach. Additionally, assessing progress is essential for communicating with other healthcare providers and ensuring continuity of care.
Step 5: Plan for Future Sessions
Outline the objectives for the next session and any modifications to the current treatment plan. This planning should be informed by the insights gained from the session summary and progress assessment. Setting clear, achievable goals for future sessions helps maintain momentum in therapy and provides the client with a sense of direction. Moreover, being proactive in planning allows for timely adjustments to the treatment plan, ensuring it remains relevant to the client's evolving needs and circumstances.
Benefits of a Psychotherapy Progress Note
Benefit | Description |
|---|---|
Consistency | Ensures uniformity in documenting client progress across sessions. |
Accuracy | Provides precise records that can be shared with other healthcare providers. |
Efficiency | Saves time by using a structured template for note taking. |
Legal Compliance | Meets documentation standards required by insurance companies and legal entities. |
Example of a Psychotherapy Progress Note
A psychotherapy progress note typically includes sections for client information, session summary, therapeutic interventions, client progress, and future session plans. This structured format helps mental health professionals maintain comprehensive and organized notes.
How to Customize a Psychotherapy Progress Note?
Customization allows therapists to tailor templates to their specific needs, incorporating unique therapeutic techniques or additional sections for group therapy notes or medication compliance. By adjusting the progress note template, mental health professionals can ensure that it aligns with the specific therapeutic interventions they employ, such as cognitive restructuring or relaxation techniques. This flexibility is particularly beneficial in group therapy settings, where the dynamics and interactions between group members might require additional documentation.
Moreover, customization can include sections dedicated to tracking the client's response to different therapeutic approaches, assessing risk factors, and noting any relevant information that could influence the treatment plan. For instance, therapists working with clients who have borderline personality disorder might add sections to document the client's motivation and any shifts in anxiety symptoms or mood.
The Evolution of Psychotherapy Progress Notes Over Time
Initially, psychotherapy progress notes were handwritten, focusing primarily on subjective observations. As digital tools became more prevalent, templates evolved to include objective data and standardized formats, improving the efficiency and accuracy of clinical documentation.
Today, digital notes offer mental health professionals the ability to store notes securely, access them easily, and share them with other healthcare providers when necessary. This evolution has greatly enhanced the therapeutic process by facilitating better communication and collaboration.
Over the years, the role of psychotherapy progress notes has expanded beyond mere documentation. They now serve as a critical component in the holistic care of clients, allowing for a comprehensive view of the therapeutic journey. These notes help in identifying patterns in a client's behavior, tracking their progress over time, and making informed decisions about future sessions. The integration of digital tools has also enabled the use of advanced analytics, providing deeper insights into the effectiveness of therapeutic interventions.
Furthermore, the evolution of progress notes has paved the way for increased accountability and transparency in mental health care. By maintaining detailed records, mental health practitioners can ensure that treatment plans are followed consistently, and any deviations are promptly addressed. This meticulous documentation is not only beneficial for client care but also essential for meeting the legal and ethical standards required in the field.
Conclusion
Psychotherapy progress note templates are indispensable tools for mental health practitioners. They ensure accurate documentation of therapy sessions, support effective treatment planning, and facilitate communication with other healthcare providers. By using structured templates, therapists can focus more on the therapeutic process and less on the administrative aspects of note taking.
For advanced solutions in medical documentation, explore our AI medical scribe services, designed to revolutionize how you create and manage your clinical notes.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

Insurance Claim Form Template
Discover practical Insurance Claim Form templates to enhance your documentation efficiency.

Mental Health Doctors Note Template
Discover practical Mental Health Doctors Note templates to enhance your documentation efficiency.

Blank SOAP Note Template
Discover practical Blank SOAP Note Template to enhance your documentation efficiency.


