
How to Write GIRP Notes: Examples & Template

Clinical documentation is vital for therapists and their clients, helping track client progress and ensure tailored, high‑quality care. GIRP notes, widely used in mental health and other healthcare fields, provide a structured format to summarize treatment plans and procedures, supporting effective client treatment.
What is a GIRP Note?
GIRP stands for Goal, Intervention, Response, and Plan. With GIRP notes, healthcare professionals such as therapists and counselors can easily organize their documentation in a way that is efficient, thorough, and aligned with the client’s unique needs, making it easier to track improvements and prepare for future sessions.
GIRP notes are a structured format of clinical documentation that initially originated in the mental healthcare field but has lately proven helpful across all areas of healthcare. The format used in these GIRP notes keeps every note clear, purposeful, and organized, helping therapists focus on what is essential and worthy of being effectively communicated regarding client progress and their subsequent future course during a session.
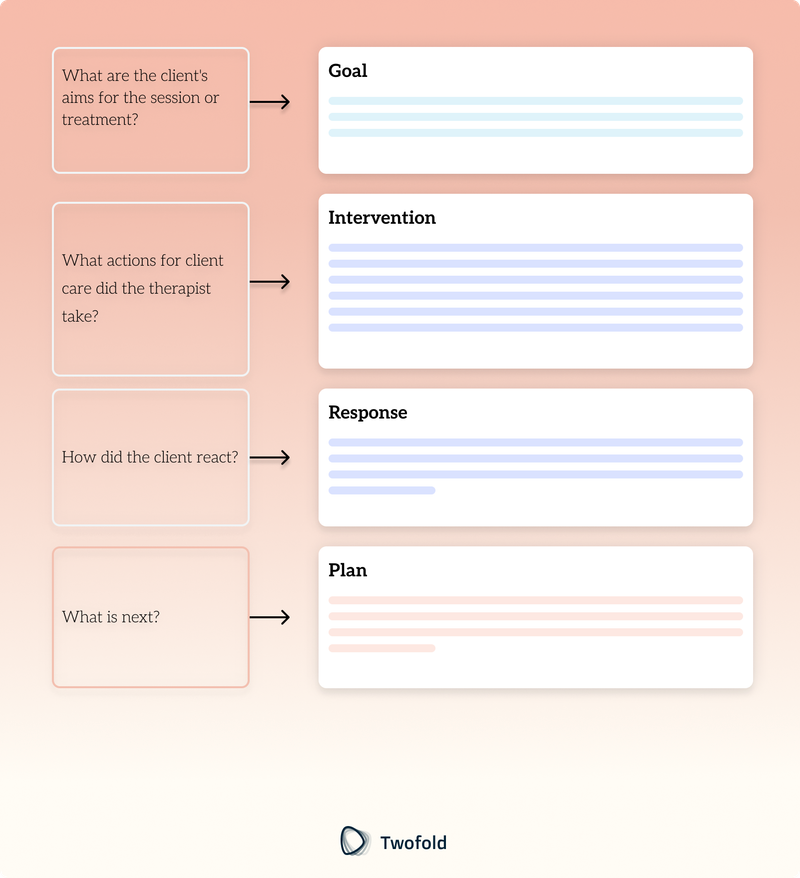
Each GIRP note has four key sections:
Sections | Focus Area | Description |
|---|---|---|
Goal | What are the client's aims for the session or treatment? | Identifies the main focus or desired outcome, such as reducing anxiety, improving mood, or enhancing specific skills. |
Intervention | What actions for client care did the therapist take? | Describes any therapeutic techniques, exercises, or guidance the provider applies during the session. |
Response | How did the client react? | Records the client’s feedback, emotions, or behavior, helping assess intervention effectiveness. |
Plan | What is next? | Outlines future steps or adjustments based on session outcomes, keeping treatment aligned with the client’s goals and progress. |
1. Goal
This section identifies the client’s aim for a specific session or treatment plan. It helps keep each session focused and purposeful, aligning with the client’s goals.
- Set Specific, Measurable Goals: The goal should be clear, achievable, and quantifiable, such as “Improve daily stress management.”
- Focus on Client-Centered Goals: Each goal should be customized to reflect the client’s unique concerns and life context. For example, for a client dealing with social anxiety, a relevant goal will be: “Develop skills to manage anxiety in social situations effectively.”
2. Intervention
In this section, the therapist records the techniques, exercises, or methods used in the session. This documentation references what was done and helps guide future treatment steps.
- Relevance to Current Needs: The interventions should be directly connected to the client’s goals and adjusted to meet evolving needs.
- Clear and Thorough Documentation: Describe each action taken to create a reliable record. For example, “Used cognitive-behavioral therapy (CBT) techniques to help challenge and reshape negative thought patterns.”
3. Response
This section captures the client’s reaction to the interventions. This can include emotions, behavioral changes, engagement levels, and other observations.
- Describe Reactions to Interventions: Note any immediate responses, including emotional shifts or changes in mood.
- Highlight Progress or Challenges: Record any significant steps forward or concerns to help shape future sessions. For example: “The client reported feeling more at ease after practicing guided breathing exercises, expressing increased motivation to try this technique independently.”
4. Plan
This section outlines the next steps based on the session’s outcomes monitoring progress. This forward‑looking approach keeps sessions consistent and helps the client build on progress.
- Summarize Goals for the Next Session: Detail any assignments or focus areas for the client to work on between sessions.
- Adjust Goals as Needed: Modify treatment as the client progresses or faces new challenges. For example: “Encourage daily relaxation practice; plan to introduce grounding exercises in the next session.”
Steps to Write Effective GIRP Notes
Here is a detailed guide on writing effective GIRP notes, ensuring all relevant information is conveyed and every aspect of the client’s case is addressed.
- Collect Comprehensive Client History: Start the evaluation process by reviewing the client's history and current circumstances to plan effective care. This may include previous medical history, treatments, life events, or other factors relevant to developing a future treatment plan.
- Set Clear, Measurable Goals: All goals should be realistic and measurable, tailored to the client's specific needs, providing clear guidance for both the client and the therapist. For example, instead of a vague goal like "improve mood," a more specific goal could be "help the client manage anxiety in social situations."
- Choose Client-Centered Interventions: When selecting interventions for treating mental health conditions, prioritize approaches that are both safe and acceptable to the client. These may include breathing exercises, stress management techniques, mindfulness practices, specific therapeutic methods, or counseling strategies that align with the client's personality and learning style.
- Create Action-Oriented Session Plans: Each session should have actionable steps for the client to complete before the next meeting. These should be manageable tasks or exercises aligned with their goals, helping foster a sense of progress and momentum. For example, if the goal is to help the client manage stress, you might suggest practicing a specific breathing exercise daily and discussing their experience in the next session.
- Regularly Assess And Adjust Progress: As the client progresses, it’s important to regularly review their goals and adjust interventions as needed. Growth is not always linear, so interventions should be flexible to accommodate the client’s responses, new developments, or emerging issues. This adaptability ensures that the care plan remains relevant and effectively supports the client’s evolving needs.
- Stay Objective: When taking notes, avoid including personal feelings, opinions, or interpretations. Focus solely on factual information, such as the client’s responses, behaviors, and activities. Refrain from speculating or making assumptions about the client’s thoughts. By maintaining clear, objective observations, you ensure your notes are professional, accurate, and useful for yourself and other healthcare providers.
Example of a Good GIRP Note
Here's a brief example of a well‑crafted GIRP note. Feel free to adjust and customize it to suit your personal style:
Goal
The client attended the session to explore effective methods for managing daily stressors. Specifically, they wanted to better understand the root causes of their stress and develop strategies for handling it in their everyday lives.
They also outlined a long‑term goal of reducing overall stress to enhance focus and well‑being, particularly in their career and other areas where stress has been a persistent challenge. This session focused on identifying practical skills the client could learn and practice independently to address these concerns.
Intervention
The therapist introduced various tools and techniques to help the client manage stress. These included guided instructions on deep breathing and progressive muscle relaxation exercises, both of which were aimed at reducing immediate tension and promoting mindfulness.
The client tried several breathing cycles, during which the therapist explained the physiological relaxation response and its benefits. Additionally, the therapist provided examples of specific situations where these techniques could be most useful, such as during a stressful workday or after a difficult commute.
Response
The client appeared focused and cooperative throughout the session, actively engaging with the therapist’s instructions. After completing the relaxation exercises, the client reported feeling significantly calmer and expressed confidence in their ability to use the techniques independently.
The client shared that the session helped them feel less anxious and more in control. While they expressed concerns about maintaining a consistent routine for these techniques at home, they also showed a positive attitude and motivation to improve their stress management skills.
Plan
The client was advised to practice relaxation techniques daily, starting with five‑minute breathing exercises in the morning and evening. The therapist also emphasized the importance of practicing during low‑stress periods to build proficiency and make the techniques more effective during high‑stress situations.
In the next session, the therapist and client will review the client’s experiences with these exercises and address any challenges. The therapist also plans to introduce additional coping strategies tailored to the client’s specific stress triggers, aiming to build a comprehensive approach to long‑term stress management.
GIRP Notes Template
For quick reference, here’s a template to streamline your GIRP notes:
- Goal: [Describe the client’s session or treatment goal]
- Intervention: [Detail the techniques or methods used to achieve the goal]
- Response: [Note the client’s reaction to each intervention]
- Plan: [Outline next steps or adjustments for future sessions]
You can use this template and copy information according to your client’s history to create a good GIRP note for yourself.
Benefits of GIRP Notes
Here is how the practice of including an effective GIRP note adds to the benefit of both mental health professionals and their clients:
- Enhanced Communication: The GIRP note format ensures every team member can easily understand and follow the client’s journey. When notes are written systematically, they promote better collaboration among healthcare providers and enhance overall client care.
- Focus on Individual Goals: The GIRP notes emphasize establishing client-specific goals for each session. These clearly defined goals ensure that every activity intentionally aligns with the client’s unique situation, increasing the treatment’s effectiveness and relevance.
- Simplified Goal Tracking: The GIRP note format emphasizes setting precise goals, allowing the clinician to identify and track the client’s progress. These goals are established in each session, providing a structured and logical framework for evaluating achievements and identifying areas where adjustments may be needed.
- Improved Progress Monitoring: Recording the client’s responses during each session simplifies tracking progress over time. This method allows both the client and clinician to observe patterns, evaluate the effectiveness of interventions, and make informed modifications to the treatment plan when necessary.
- Supports Treatment Plans: GIRP notes provide a clear roadmap and support a collaborative, cohesive, and fully integrated treatment model. This ensures that all therapeutic interventions align with the client’s overarching treatment goals and objectives.
- Clear Documentation: Using a standardized format for documentation ensures clarity, which is significant for effective collaboration among medical staff and improving communication between the therapist and the client.
Common Mistakes to Avoid in GIRP Notes
Mistakes in GIRP notes can disrupt communication, misrepresent progress, and impact care quality. Here are the common mistakes and key tips to avoid them:
Mistakes | Description | Example/Advice |
|---|---|---|
Vague Goals | Goals should be clear, specific, and measurable. | Avoid “feel happy”; instead, use “decrease social anxiety.” |
Inconsistent Updates | Periodic updates are essential for precise tracking of progress. | Ensure every session has updated notes. |
Generic Responses | Capture specific client responses to interventions rather than generic summaries. | Replace “client reacted positively” with specific details. |
Incomplete Documentation | Document all interventions and avoid skipping important details that may affect future sessions. | Record actions comprehensively. |
Unclear Plans | Clearly outline the next steps to maintain focus and continuity in treatment. | Include assignments or goals for the next session. |
Best Practices for Effective GIRP Notes
Here are a few important pointers to keep in mind:
- Set a Time Limit: Keep note-taking efficient by setting a time limit or allocating a fixed amount of minutes per note. This approach enhances focus on key details, ensures effectiveness, and reduces time spent searching for information.
- Be Concise: Avoid irrelevant details and use clear, direct language to highlight key observations, actions, and outcomes. Concise notes ensure easy understanding and quick reference for your team members.
- Leverage AI and Tech Tools: Use digital tools and AI software to streamline your work. Templates, auto-population, and triggers maintain standards, reduce revisions, and save time on session-specific details and documentation checks.
- Perform a Quick Review: Quickly check for omissions, errors, or unclear concepts to ensure the information is accurate and suitable for team use. A fast scan can catch minor mistakes that might affect record integrity.
- Improve Through Practice: The more you use the GIRP format, the easier and more efficient note-taking becomes, helping you create faster, more targeted and effective records.
- Use Templates: Standardized templates ensure notes follow the GIRP format, reducing oversights and promoting consistency with a clear, easy-to-fill structure.
GIRP vs Other Note Formats
GIRP notes differ from other formats like BIRP, PIRP, SOAP, and DAP. Each has unique structures, and providers may choose one based on their specific documentation style or client needs. A concise outline is given below:
Note Formats | Structure | Focus | Best Suited For |
|---|---|---|---|
GIRP (Goal, Intervention, Response, Plan) | Goal-oriented and tracks client response to interventions | Centers on setting and achieving client-specific goals | Practitioners who prioritize structured progress tracking |
BIRP (Behavior, Intervention, Response, Plan) | Focuses on observable client behavior, followed by interventions and client response | Starts with behavioral observations, leading to intervention and planning | Therapists focused on behavioral therapy and tracking actions |
PIRP (Problem, Intervention, Response, Plan) | Begins by identifying a problem, then follows with intervention and response | Highlights problem identification for session-specific issues | Sessions focused on problem-solving and targeted interventions |
SOAP (Subjective, Objective, Assessment, Plan) | Combines subjective client input with objective observations and assessment | Provides a comprehensive view of both mental and physical aspects | Healthcare providers requiring a holistic approach to care |
DAP (Data, Assessment, Plan) | Briefly documents observations, clinician’s assessment, and plans | Ideal for short or single-session notes with focused goals | Short-term interactions or when concise notes are needed |
How AI Can Enhance GIRP Note-Taking
Artificial Intelligence (AI) streamlines documentation, helping healthcare providers manage large volumes of client data and notes efficiently.
Here is how AI can enhance writing GIRP notes:
- Automating Repetitive Sections: AI saves time on documentation by auto-filling standard fields and suggesting phrases based on prior notes, like frequently used therapeutic techniques.
- Prompts for Consistent Documentation: AI tools guide providers through the GIRP framework, ensuring no details are missed, offering valuable support for new providers or busy shifts.
- Templates and Structured Outlines: AI tools offer customizable GIRP templates, ensuring consistent, time-saving documentation that supports quality, continuity, and easy review by other providers.
GIRP Notes with Twofold
Writing detailed GIRP notes is crucial for effective patient care but can often be a time‑consuming task for clinicians. Twofold, an innovative AI scribe designed specifically for healthcare professionals, streamlines this process by automating the creation of GIRP notes. Leveraging advanced natural language processing, Twofold transcribes patient interactions in real‑time and intelligently organizes the information into the Goal, Intervention, Response, and Plan sections. This ensures that your documentation is thorough, accurate, and compliant with industry standards. With Twofold handling the administrative workload, clinicians can focus more on providing quality care and less on paperwork, enhancing both efficiency and patient outcomes.
Conclusion
GIRP notes are an invaluable tool for structured, consistent documentation in healthcare. They enhance client care, help establish clear communication, and create a reliable record of progress. Using the GIRP format, providers can focus on meaningful goals and support lasting improvements in treatment outcomes.
Disclaimer
All mental health documentation examples are entirely fictional and intended for informational use only.
Frequently Asked Questions
ABOUT THE AUTHOR
Dr. Andleeb Asghar
Research Collaborator
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

Top AI SOAP Note Tools in 2026 (Tested by Real Clinicians)
Discover Top AI SOAP Note Tools in 2026 - tested by real clinicians. Compare accuracy, EHR integrations, HIPAA/BAA, pricing, and use cases to pick the best fit.
What Makes Medical AI Notes Apps Actually Safe to Use?
Adopting AI notes is tempting, but is it safe? Here is a breakdown of non-negotiable features that truly protect your patients and your practice

Best Reviewed AI Medical Scribe (2026) – According to Clinicians
See why clinicians rate these 7 AI scribes highest in 2026. Compare rankings, real‑world reviews, pricing and HIPAA safeguards to find the best AI scribe for you.

