
90792 CPT Code: Guide to Psychiatric Diagnostic Evaluation With Patient, Including Medical Services

Key Takeaways
- CPT Code 90792 is essential for comprehensive psychiatric evaluations, requiring licensed mental health professionals to conduct detailed assessments and follow strict documentation guidelines for accurate billing.
- Accurate time documentation (60 to 120 minutes) is critical for billing under CPT Code 90792, ensuring thorough evaluations and appropriate compensation for services rendered.
- Reimbursement rates for CPT Code 90792 can vary significantly among payers, with Medicare offering higher rates; providers must remain informed about these rates for effective practice management and billing strategies.
CPT Code 90792 is used for billing comprehensive psychiatric diagnostic evaluations by licensed mental health providers. In this article, you’ll learn about the main components, documentation practices, and billing tips related to the 90792 CPT code to ensure proper reimbursement.
Understanding CPT Code 90792
CPT Code 90792 refers to a Psychiatric Diagnostic Interview Examination. This examination is carried out by a licensed mental health provider. This code is pivotal in conducting comprehensive psychiatric assessments that help understand a patient’s mental health needs and develop tailored treatment plans. CPT Code 90792 facilitates psychiatric evaluations and billing for associated services, ensuring compensation for mental health professionals’ expertise and time.
The psychiatric diagnostic evaluation under CPT 90792 involves a thorough medical and psychiatric history, mental status examination establishment, initial diagnosis evaluation, psychiatric diagnosis interview examination, evaluation of treatment response, and the creation of an initial treatment plan. These components are crucial in forming a complete picture of the patient’s mental health, encompassing family and social aspects to provide a holistic approach to treatment. The mental status examination assesses the patient’s cognition, emotions, and overall mental functioning, which forms the basis for determining the initial diagnosis and treatment strategy.
Documentation for CPT Code 90792 must include comprehensive medical assessments and any additional psychiatric evaluations conducted to ensure accurate representation of the evaluation. Proper documentation is not just a bureaucratic necessity but a critical aspect of patient care, ensuring continuity and clarity in treatment.
The detailed gathering of medical and psychiatric history, including family and social aspects, helps in creating a robust and effective treatment plan for mental health clients, aligning with the best practices in mental health care.
Key Requirements for Billing CPT Code 90792
Billing for CPT Code 90792 is not a straightforward task; it requires adherence to several key procedural requirements.
Only licensed mental health providers are eligible to bill under this code, ensuring that the evaluations are conducted by professionals with the necessary expertise.
The procedural requirements include:
- Conducting a detailed complete medical history
- Performing a thorough examination
- Establishing an initial diagnosis
- Evaluating the patient’s ability to respond to treatment
- Developing a comprehensive treatment plan
These steps are essential to ensure that the evaluation is thorough and meets the standards required for billing.
Another critical aspect of billing CPT Code 90792 is the documentation of time spent during the evaluation. Accurate time documentation is necessary for proper billing and reimbursement, as it reflects the effort and dedication put into each patient’s assessment. This ensures that the billing process is transparent and that the healthcare provider is appropriately compensated for their time and expertise.
Maintaining detailed and accurate records is not just about compliance but also about providing high‑quality care. Each element of the evaluation, from the medical history to the treatment plan, must be meticulously documented to support the billing process and ensure that the patient receives the best possible care. This thorough approach helps in building a robust patient record that can guide future treatments and interventions. By adhering to these practices, healthcare providers can optimize their use of the 90792 CPT code, ensuring accurate billing and comprehensive patient care.
Time Allocation for CPT Code 90792
Time allocation is a crucial factor when billing for CPT Code 90792. The required duration for conducting a psychiatric diagnostic evaluation under this code ranges from 60 to 120 minutes. This time frame allows for a thorough assessment of the patient’s mental health status, ensuring that all necessary components of the evaluation are adequately covered. Billing for CPT Code 90792 necessitates a minimum of 60 minutes, with a maximum of 120 minutes for the diagnostic interview.
Allocating 60 to 120 minutes for the evaluation enables a detailed exploration of the patient’s mental health, including their medical and psychiatric history, mental status examination, and initial diagnosis. This time frame is essential to ensure that the evaluation is comprehensive and meets the criteria for billing. It is also important to ensure that the evaluation duration aligns with the service components performed to meet the billing criteria.
Scheduling these evaluations within regularly scheduled office hours or during evening or holiday office hours can help in managing time effectively. Ensuring that the time spent on each evaluation and management services is documented accurately is crucial for reimbursement and for maintaining the integrity of the billing process.
This approach helps avoid discrepancies and ensures appropriate compensation for healthcare providers’ time and effort.
Reimbursement Rates for CPT Code 90792
Understanding reimbursement rates for CPT Code 90792 is essential for effective billing and ensuring that mental health professionals are fairly compensated. Reimbursement rates for this code can vary significantly from year to year and by payer, making it crucial for providers to stay informed about the latest rates. For instance, the reimbursement amount for CPT Code 90792 has fluctuated over the years, with rates such as $196.55 in 2023, $201.68 in 2021, and $218.90 in 2022.
Medicare typically reimburses psychiatrists at higher rates compared to other insurers, reflecting the value placed on comprehensive psychiatric evaluations. Staying informed about these rates is essential to ensure accurate billing and appropriate compensation. This knowledge helps healthcare providers plan their services and billing strategies effectively, optimizing their reimbursement outcomes.
Regularly checking the reimbursement rates with individual insurance payers is critical, as these rates can differ significantly. This proactive approach helps in maintaining financial stability and ensuring that the services provided are adequately compensated. Staying updated on reimbursement rates helps mental health professionals manage their practices better and provide high‑quality care.
2023 Reimbursement Rates
In 2023, the reimbursement rate for CPT Code 90792 is $196.55, reflecting the financial compensation for this specific code. This rate highlights the importance of comprehensive psychiatric evaluations and the need for proper documentation and billing practices. Verifying specific reimbursement rates with each insurance payer is crucial, as these rates can differ significantly.
Ensuring that the billing aligns with these rates helps in maximizing reimbursement and maintaining the financial health of the practice.
License Level Requirements for CPT Code 90792
Billing for CPT Code 90792 is restricted to licensed medical professionals, such as psychiatrists and physicians, due to the comprehensive medical assessment required. Only licensed MDs or DOs are permitted to bill for this code, distinguishing it from CPT Code 90791, which does not require a medical assessment. This higher license level requirement ensures that the evaluations are conducted by professionals with the necessary expertise to perform an accurate and thorough assessment.
The medical assessment component is a critical aspect of CPT Code 90792, limiting its use to licensed physicians or psychiatrists. This requirement emphasizes the importance of a detailed and accurate medical evaluation in the diagnostic process. The distinction between CPT Code 90792 and similar codes like CPT Code 90791 lies in this medical assessment component, which necessitates a higher level of licensure and expertise.
Reimbursement for CPT Code 90792 is influenced by the medical assessment component, further emphasizing the need for licensed physicians to conduct these evaluations. This ensures that the evaluations meet the high standards required for billing and that the providers are appropriately compensated for their expertise and time. Understanding these license level requirements is essential for accurate billing and effective practice management.
Add-On Codes Enhancing CPT Code 90792 Billing
Add‑on codes play a significant role in enhancing the billing process when used alongside CPT Code 90792. These codes reflect additional services or complexities in psychiatric evaluations, ensuring that all aspects of the service provided are captured and reimbursed. The purpose of these add‑on codes is to document interactive complexity and any supplementary services provided during the evaluation.
Specific add‑on codes that can be used with CPT Code 90792 include:
These codes help in capturing the full scope of the services provided, ensuring that the billing is comprehensive and accurate. These add‑on codes help mental health professionals get compensated for the complexity and extra time involved in evaluations.
Understanding and utilizing these add‑on codes effectively can significantly enhance the billing process, optimizing reimbursement outcomes. This approach helps in accurately reflecting the services provided and ensures that the healthcare provider’s efforts are adequately rewarded. Incorporating these codes allows mental health professionals to provide high‑quality care and maintain financial stability.
Interactive Complexity: CPT Code 90785
CPT Code 90785 is an add‑on code that indicates additional communication factors complicating the evaluation. This code is used to address complexities in certain psychiatric evaluations, such as communication challenges due to non‑verbal behavior, intellectual impairments, or emotional issues. These conditions may necessitate the use of the interactive complexity add‑on code, ensuring that the additional time and cognitive effort involved in the evaluation are documented and reimbursed.
The use of CPT Code 90785 allows for accurate documentation of the complexities involved in the evaluation, ensuring that the healthcare provider is compensated for the extra effort required. This code is particularly useful in cases where the patient’s condition requires more time and specialized communication techniques, reflecting the true nature of the services provided.
Incorporating CPT Code 90785 into the billing process ensures that the evaluation is fully documented, capturing all aspects of the patient’s condition and the provider’s efforts. This approach helps in optimizing reimbursement and maintaining the financial health of the practice, while also ensuring high‑quality care for the patient.
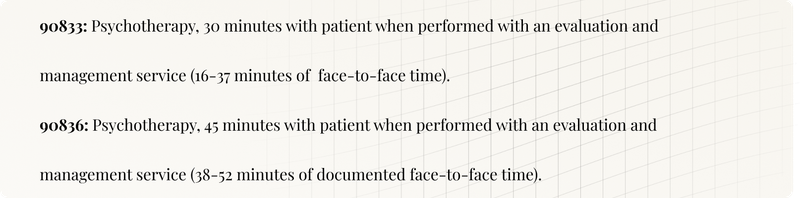
Additional Services: CPT Codes 90833 and 90836
CPT Code | Description | Purpose | Benefits |
|---|---|---|---|
90833 | Add-on code for therapy sessions provided during diagnostic evaluations. | Captures additional therapy time during evaluations. | Ensures full scope of services is documented and reimbursed. |
90836 | Add-on code for therapy sessions provided during diagnostic evaluations. | Captures additional therapy time during evaluations. | Ensures full scope of services is documented and reimbursed. |
These codes are used to document supplementary medical services provided during evaluations. Incorporating these codes ensures all aspects of the evaluation are captured.
Proper Use of Billing Modifiers for CPT Code 90792
Proper use of billing modifiers is crucial when billing for CPT Code 90792. Billing modifiers must accurately reflect the clinician’s qualifications, which is essential for proper reimbursement. These modifiers indicate the provider type and ensure that the billing process is transparent and meets the payer’s requirements.
Using incorrect billing modifiers for 90792 CPT code can result in claim denials or payment delays, significantly impacting the financial stability of a practice. Payers have specific guidelines regarding billing modifiers, and it is essential to review these guidelines before submission to ensure compliance. This diligence helps in avoiding common pitfalls and ensures that the billing process is smooth and efficient.
Maintaining specific documentation rules for both codes and modifiers is essential to ensure compliance and increase reimbursement success. By adhering to these guidelines, mental health professionals can optimize their billing practices for 90792 CPT code, ensuring that they are compensated for their services accurately and promptly. This approach helps in maintaining the financial health of the practice while providing high‑quality care to patients through comprehensive psychiatric diagnostic evaluations. The proper application of modifiers enhances the billing process, ensuring the 90792 CPT code is used effectively in psychiatric diagnostic evaluations, thereby optimizing reimbursement outcomes.
Step-by-Step Guide to Billing CPT Code 90792
Billing for CPT Code 90792 involves several critical steps, starting with the accurate completion of the CMS‑1500 form. This form is used for insurance billing and must be filled out meticulously to avoid errors. CPT Code 90792 should be added to line 24 on the CMS‑1500 form, ensuring that it is clearly indicated for proper processing.
Using specific billing modifiers such as AJ, AF, AH, or HP is essential to indicate the provider’s credentials when billing for CPT Code 90792. These modifiers help in reflecting the provider’s qualifications and ensuring that the billing is accurate and meets the payer’s requirements. Thorough documentation and accurate patient identification details are crucial to avoid claim denials or lower payments.
Following this guide helps mental health professionals maintain efficient and compliant billing practices. This approach helps in optimizing reimbursement outcomes and maintaining the financial stability of the practice. Accurate billing is not just about getting paid but also about ensuring that the services provided are fully documented and recognized.
Medicaid and Medicare Reimbursement Insights
Medicare reimbursement for CPT Code 90792 has consistently been higher than for other payers, reflecting the value placed on comprehensive psychiatric evaluations. Medicare typically permits billing for diagnostic evaluations once per year, emphasizing the importance of precise coding and documentation. This policy highlights the need for accurate and thorough evaluations to ensure that the billing process is smooth and that providers are fairly compensated.
Medicaid reimbursement rates for CPT Code 90792 are determined by individual state fee schedules, leading to significant variability in rates. For example, the reimbursement rate in Mississippi is approximately $134.42, whereas in New Jersey, it is $325.00. Providers must consult specific state Medicaid fee schedules to identify the exact reimbursement rates for CPT Code 90792.
Understanding these reimbursement insights is crucial for effective billing and practice management. By staying informed about the reimbursement rates and policies of Medicare and Medicaid, mental health professionals can optimize their billing practices and ensure that they are adequately compensated for their services. This approach helps in maintaining the financial health of the practice while providing high‑quality care to patients.
Resources for Mental Health CPT Codes
There are various resources available for understanding mental health CPT codes, which can significantly assist mental health professionals in their billing practices. Comprehensive billing guides covering various mental health codes are available, providing detailed information and practical tips for effective billing. The AMA offers a behavioral health coding guide that lists key CPT codes for various behavioral health services, helping practitioners navigate the complexities of billing.
The Behavioral Health Integration Compendium provides actionable information for health care organizations on delivering integrated behavioral care, ensuring that all aspects of mental health services are covered. Additionally, the BHI webinar series offers training and resources focused on behavioral health integration, providing valuable insights and practical tips for practitioners.
Strategic behavioral health guides assist in optimizing patient care within mental health settings, helping behavioral health providers navigate the complexities of billing and optimize reimbursement. Utilizing these resources helps mental health professionals enhance billing practices, ensure compliance, and maximize reimbursement outcomes. This approach helps in maintaining the financial health of the practice while providing high‑quality care to patients.
Case Study: Successful Billing Practices
Effective coding and billing practices are essential for optimizing reimbursement outcomes for CPT Code 90792 whether for in‑person or tele-health sessions. Practitioners may bill both 90791 and 90792 on the same day if different providers conduct the evaluations and payer policies allow it. Understanding payer policies is crucial in facilitating effective billing strategies that maximize reimbursement potential. This knowledge helps in navigating the complexities of billing and ensuring that the services provided are fully recognized and compensated.
Adopting these effective billing practices and using AI assisted tools like Twofold Health can lead to significantly higher reimbursement outcomes for mental health providers. By implementing best practices and staying informed about payer policies, mental health professionals can optimize their billing strategies, ensuring that they are adequately compensated for their services. This approach helps in maintaining the financial health of the practice while providing high‑quality care to patients.
Summary
In summary, mastering CPT Code 90792 is essential for any mental health professional involved in psychiatric evaluations and insurance billing. Understanding the key requirements, time allocations, reimbursement rates, and proper use of billing modifiers is crucial for effective billing practices. Utilizing add‑on codes and following a step‑by‑step guide to billing can significantly enhance reimbursement outcomes.
Medicaid and Medicare reimbursement insights highlight the importance of staying informed about specific payer policies and rates. Various resources are available to assist mental health professionals in navigating the complexities of billing, ensuring compliance and optimizing reimbursement. Effective billing practices, as demonstrated in the case study, can lead to higher reimbursement outcomes and financial stability.
By implementing the tips and insights provided in this blog post, mental health professionals can optimize their billing practices, ensuring that they are fully compensated for their services. This approach helps in maintaining the financial health of the practice while providing high‑quality care to patients. Embrace these practices and take your billing efficiency to new heights.
Enhance your practice with an AI medical scribe to streamline documentation and improve patient care.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

F33.1 ICD-10 Code: Major Depressive Disorder
Discover essential insights on the F33.1 ICD-10 Code code for health professionals. Enhance your practice and navigate billing with confidence.

99403 CPT Code: Preventive Medicine Counseling, 45 minutes
Discover essential insights on the 99403 CPT Code for health professionals. Enhance your practice and navigate billing with confidence.

90899 CPT Code: Unlisted Psychiatric Service or Procedure
Discover essential insights on the 90899 CPT Code for health professionals. Enhance your practice and navigate billing with confidence.

