
Clinical Note Template
In today's fast‑paced medical environment, efficient and accurate record‑keeping is essential for providing excellent patient care. Medical professionals are constantly seeking ways to streamline their workflows without compromising on the quality of care they provide. One effective solution is the use of a clinical note for recording patient encounters. These notes not only save time but also ensure that all critical information is documented consistently across different healthcare settings.
Effective documentation plays a crucial role in the continuity of care, legal compliance, and communication among medical teams. By adopting a structured clinical note template, practitioners can focus more on their patients and less on administrative burdens. This comprehensive guide explores the essential elements of a clinical note template, how to implement it in your practice, and the significant advantages it offers.
Try Out Our Clinical Note Templates
Enhance your practice by trying our customizable clinical note templates here. These clinical note templates are designed to meet the diverse needs of various medical specialties, ensuring your clinical notes are thorough, accurate, and compliant with legal standards.
What Is a Clinical Note Template?
A clinical note template is a structured framework designed to assist medical professionals in systematically documenting patient encounters. It provides a consistent format to record all vital information, such as the patient’s medical history, current condition, assessment, and treatment plan. By using a progress note template, practitioners can streamline the documentation process, ensuring that key details are captured efficiently while reducing the time spent on paperwork. This allows more focus on delivering quality patient care and enhances overall efficiency in healthcare settings.
Understanding Clinical Notes and Their Role
Clinical notes are comprehensive records that document every aspect of a patient’s interaction with healthcare providers. These notes play a critical role in ensuring high‑quality care and serve multiple important purposes:
- Continuity of Care: Clinical notes, particularly those created using standardized progress note templates, ensure that all healthcare providers involved in a patient’s treatment have a clear understanding of the patient’s status and treatment history. This continuity is especially important in complex cases or when care is transferred between providers because they accurately capture patient's medical history.
- Legal Protection: Detailed clinical notes provide legal evidence of the care and services rendered. A well-structured progress note created with a clinical note template ensures thorough documentation, which can be crucial in legal or compliance-related situations.
- Billing and Insurance: Accurate and detailed documentation is essential for proper coding and reimbursement. Using standardized progress note templates makes it easier to meet insurance requirements and ensures clarity in billing, reducing the risk of disputes or claim denials.
The Role of Clinical Note Templates in Streamlining Documentation
Clinical note templates standardize the creation of clinical notes, making the documentation process more consistent, efficient, and accurate. Whether documenting routine visits or specialized treatments, progress notes generated with these templates ensure that essential information is recorded systematically. This not only enhances the quality of patient care but also supports practitioners in meeting legal, compliance, and administrative requirements.
By utilizing clinical notes, healthcare professionals can ensure that their documentation meets professional standards while freeing up more time to focus on patient care.
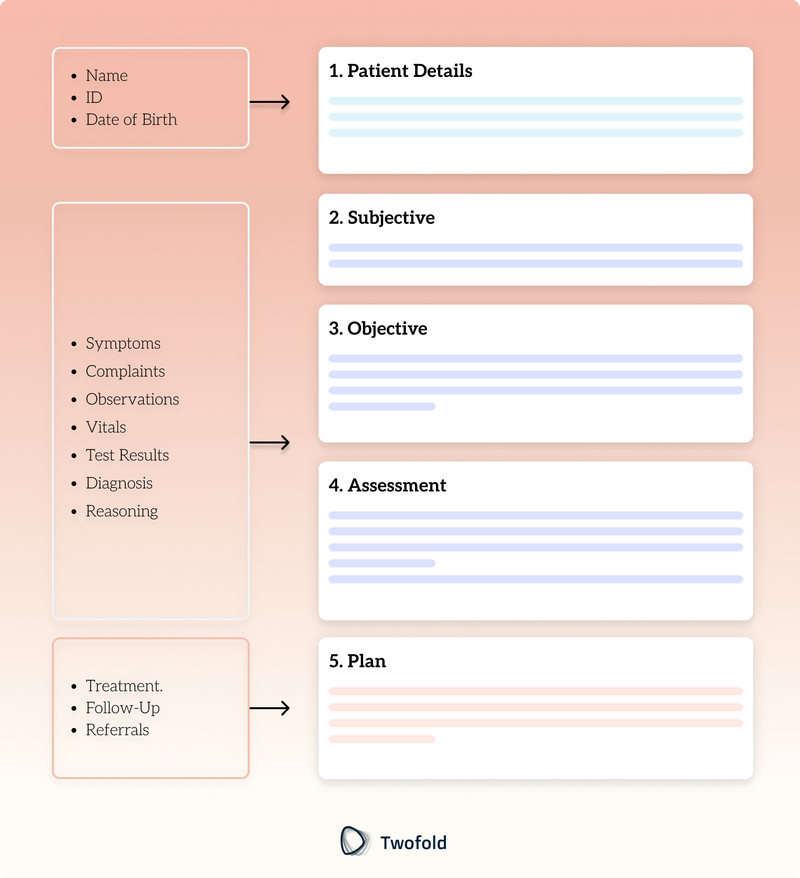
Key Components of a Clinical Note Template
An effective clinical note template includes several essential components:
1. Patient Details
Accurate patient details are crucial to link the clinical notes to the correct records, ensuring that the patient's medical treatment is based on precise information. This includes:
- Name
- Identification Number (ID)
- Date of Birth (DOB)
2. Subjective (Symptoms and Complaints)
This section captures the patient's description of their symptoms and concerns, providing insight into their patient's medical condition. It includes:
- Symptoms: Patient-reported issues such as pain or discomfort.
- Complaints: Specific concerns prompting the medical visit.
In mental health settings, this also encompasses observations relevant to mental health progress, crucial for writing notes.
3. Objective (Observations, Vitals, Test Results)
Practitioners record measurable data obtained during the physical examination and diagnostic tests. This section covers:
- Observations: Clinician's findings during the examination.
- Vitals: Blood pressure, heart rate, temperature, etc.
- Test Results: Lab tests and imaging studies.
4. Assessment (Diagnosis and Reasoning)
Combining subjective and objective data to formulate a diagnosis, including:
- Diagnosis: Identified medical condition.
- Reasoning: Rationale behind the diagnosis.
5. Plan (Treatment, Follow-Up, and Referrals)
Outlining the next steps in the patient's medical treatment, such as:
- Treatment: Medications or interventions planned.
- Follow-Up: Future appointments or monitoring.
- Referrals: Recommendations to specialists.
The Importance of Clinical Notes in Healthcare
Clinical notes are essential in the healthcare industry, serving as the backbone of communication among healthcare practitioners. They ensure that everyone involved in a patient's care is informed and aligned, fostering better outcomes. Utilizing structured tools like a clinical note template can significantly enhance the quality of documentation, particularly for tasks such as writing therapy progress notes and creating notes in the mental health industry.
Enhancing Patient Safety
Detailed and accurate clinical notes are critical in preventing medical errors. They provide complete and precise information about the patient's history, current condition, and treatment plans, reducing the risk of miscommunication. Using standardized progress note templates ensures that all necessary details are captured systematically, which is particularly crucial for mental health progress notes, where nuances in a patient’s condition can significantly impact treatment outcomes.
Supporting Decision-Making
Clinicians depend on comprehensive progress notes to make informed decisions about diagnoses, treatment plans, and follow‑ups. A well‑organized clinical note template ensures that no critical data is overlooked, streamlining the process of writing the notes. This is particularly beneficial in mental health care, where thorough and clear documentation can guide effective interventions and adjustments to therapy.
Facilitating Research and Education
Clinical notes serve as valuable resources for medical research, helping identify trends and informing evidence‑based practices. In educational settings, structured progress note templates can be instrumental in teaching healthcare providers how to create effective mental health progress notes and other forms of documentation. This supports the development of competent practitioners who are skilled in maintaining high‑quality clinical records.
By leveraging structured documentation practices, healthcare providers can enhance communication, improve patient outcomes, and support the broader goals of research, education, and compliance in the medical field.
How to Use Clinical Note Templates: Step-by-Step Process
Implementing a clinical note template enhances efficiency and accuracy. Here's how to effectively integrate them into your practice:
Step 1: Access and Save the Template
- Download: Obtain the appropriate clinical note template for your specialty, including progress note templates for specific needs.
- Customize: Adjust the template to suit your practice's specific requirements.
Step 2: Fill Out After Patient Encounters
- Timeliness: Complete the clinical notes immediately after the visit to ensure accuracy.
- Detail: Include all relevant information, avoiding omissions.
Step 3: Review and Correct Errors
- Proofread: Check for mistakes or inconsistencies.
- Clarity: Ensure that other healthcare practitioners can understand the clinical notes.
Step 4: Store Securely (Legal and HIPAA-Compliant Practices)
- Security: Use compliant systems to protect patient information.
- Access Control: Limit access to authorized personnel only.
Benefits of Clinical Note Templates
Using a structured clinical note template offers several advantages, especially when documenting a therapy progress note:
Save Time While Maintaining Precision
Clinical note templates streamline the documentation process, enabling practitioners to focus more on client care. By providing a consistent structure, they reduce the likelihood of errors and ensure no critical information is overlooked. This is particularly valuable when creating a detailed therapy progress note that need to balance thoroughness and efficiency.
Enhance Team Collaboration Through Clear Documentation
Standardized clinical note templates improve communication among healthcare practitioners. When everyone uses the same format, it becomes easier to understand and follow patient records, facilitating seamless transitions and collaborative care. This consistency is especially beneficial in scenarios like group therapy or multidisciplinary teams, where clear and structured therapy notes (or group therapy notes) are crucial for effective coordination.
Ensure Legal and Insurance Compliance
Comprehensive documentation is essential for legal protection and accurate billing. Clinical note templates ensure that all necessary details are included, aiding compliance with legal requirements and insurance policies. A well‑documented therapy progress note not only support reimbursement claims but also provide a reliable record in case of audits or disputes.
Conclusion
Efficient and accurate documentation is a cornerstone of effective patient care. By adopting structured clinical note templates, healthcare practitioners can ensure that all critical information is captured consistently, enhancing both individual patient outcomes and overall quality healthcare. These clinical note templates not only streamline administrative tasks but also facilitate better communication among care teams and compliance with legal and insurance requirements.
In an era where healthcare demands are continually increasing, leveraging tools like clinical note templates is essential. It allows practitioners to devote more time and attention to their patients, which is the ultimate goal of any healthcare provider. Whether you're a general practitioner, a specialist, or a mental health professional, integrating standardized clinical note templates into your practice can make a significant difference.
By focusing on the human aspect of care while utilizing efficient documentation methods, healthcare providers can achieve a balance that benefits both the practitioner and the patient. The adoption of a clinical note template is not just a matter of convenience but a step towards improving the overall standard of care.
For advanced solutions in medical documentation, explore our AI medical scribe services, designed to revolutionize how you create and manage your clinical notes.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.

Elad Maymon
Elad is a seasoned professional with extensive experience in the health tech sector, specializing in software development and project management. He has played pivotal roles in various organizations, contributing to the successful delivery of innovative healthcare solutions. Elad's expertise includes developing and implementing health‑focused software platforms, ensuring compliance with industry standards, and integrating advanced technologies to enhance patient care. His commitment to leveraging technology to improve healthcare outcomes underscores his dedication to the field.
- Use Standard Medical Terminology: Enhances clarity and consistency across clinical notes.
- Leverage Technology: Utilize digital tools and software designed for the documentation process.
- Regular Updates: Keep your clinical note templates current with medical standards and regulations.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

Therapy Session Notes Template
Discover practical Therapy Session Notes templates to enhance your documentation efficiency.

Wellness Wheel Template
Discover practical Wellness Wheel templates to enhance your documentation efficiency.

SOAP Note Template
Discover practical SOAP Note templates to enhance your documentation efficiency.



