
SOAP Note Template
Writing medical notes can sometimes feel like piecing together a puzzle, especially when different formats and requirements come into play. If you’ve ever felt overwhelmed by jargon or unsure of what to include, you’re not alone. Having a structured approach, like the SOAP note template, can make all the difference in your documentation process. This article will break down the SOAP note template into digestible parts, so you can tackle those notes with confidence.
What Is a SOAP Note Template?
A SOAP note template is a structured method for documenting patient encounters, commonly used in medical settings. The acronym stands for Subjective, Objective, Assessment, and Plan, guiding healthcare professionals in capturing important information effectively.
This template promotes clarity and consistency in medical documentation, ensuring that records are thorough and precise. It allows for an organized approach to patient evaluation, which can facilitate better treatment outcomes and communication among healthcare providers.
Key Components of a SOAP Note Template
Each SOAP note should include clear sections to convey critical information efficiently.
- Subjective: Patient's reported symptoms, feelings, and statements.
- Objective: Measurable data, including vital signs and physical examination findings.
- Assessment: The clinician's interpretation of the subjective and objective data.
- Plan: Proposed treatment plan, including medication, education, or follow-up appointments.

How to Use a SOAP Note Template: Step-by-Step Process
- Begin with the patient's information, including name and date of visit.
- In the Subjective section, enter the patient’s complaints and relevant history.
- In the Objective section, document examination results and any measurable data.
- Conduct your Assessment based on the information collected.
- Formulate a Plan for treatment and follow-up care.
- Review your completed note for accuracy and completeness before saving or sharing.
Benefits of a SOAP Note
Benefit | Description |
|---|---|
Improved Communication | Facilitates clearer interaction among healthcare providers. |
Standardization | Provides a consistent format for all medical records. |
Enhanced Patient Care | Encourages comprehensive assessments and individualized treatment plans. |
Legal Protection | Accurate documentation can help prevent legal issues. |
Time Efficiency | Streamlines the documentation process, saving time in busy practices. |
Stakeholders in SOAP Notes
Several stakeholders benefit directly from the effective use of SOAP notes.
- Healthcare Providers: Doctors and nurses rely on SOAP notes for clear records that enhance coordination of care.
- Patients: Clear documentation leads to better communication and understanding of their care plans.
- Insurance Companies: Requires proper documentation for claims processing and reimbursement.
- Legal Professionals: Maintain accurate records that can be crucial in medical liability cases.
Example of a SOAP Note
Here's a succinct example illustrating the SOAP note format:
Real-World Use Cases: Practical Impact of the SOAP Note Template
The SOAP note template showcases its efficiencies across various healthcare scenarios.
- Nurse in Emergency Room: In a busy ER, a nurse quickly documents patient vitals using the objective section, allowing doctors to make informed decisions swiftly.
- Primary Care: A primary care physician uses the assessment part to summarize a patient’s chronic conditions, making it easier to strategize for upcoming visits.
- Therapy: A physiotherapist documents a patient's progress in rehabilitation through the plan section, facilitating continuity of care across sessions.
- Legal: During a legal dispute, a well-documented SOAP note serves as a key piece of evidence demonstrating that proper protocols were followed during a patient's treatment.
Conclusion
This article outlined the components and importance of the SOAP note template in medical documentation. The structured approach enhances communication, fosters standardized documentation, and ultimately improves patient care. By following the outlined steps and best practices, healthcare professionals can create effective SOAP notes that streamline their clinical workflows.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.

Dr. Danni Steimberg
Dr. Danni Steimberg is a pediatrician at Schneider Children’s Medical Center with extensive experience in patient care, medical education, and healthcare innovation. He earned his MD from Semmelweis University and has worked at Kaplan Medical Center and Sheba Medical Center.
- In advanced clinical practice, SOAP Notes transcend a standard checklist. They become a dynamic blueprint, capturing nuanced shifts, enabling immediate treatment adaptations, and laying the foundation for lasting patient progress.
- Subjective: Capture Vivid Patient Narratives
Rather than noting “patient reports headache,” prompt descriptions like “sharp pain behind the eyes, worsens with bright lights.” These rich, sensory details illuminate potential triggers and guide more precise diagnostic pathways. - Objective: Leverage High-Level Metrics
Move beyond basic vitals by including validated scales (e.g., PHQ-9), digital trackers, or advanced imaging. This data-driven approach builds a robust record that justifies interventions and fosters transparent clinical decision-making.
Assessment & Plan: Create Personalized Progress Maps
Go further than a generic treatment outline—detail medication changes, integrative therapies, and timelines for follow‑up. This roadmap not only tracks progress step‑by‑step but also stands strong under peer review and insurance scrutiny.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

Living Well Template
Discover practical Living Well templates to enhance your documentation efficiency.
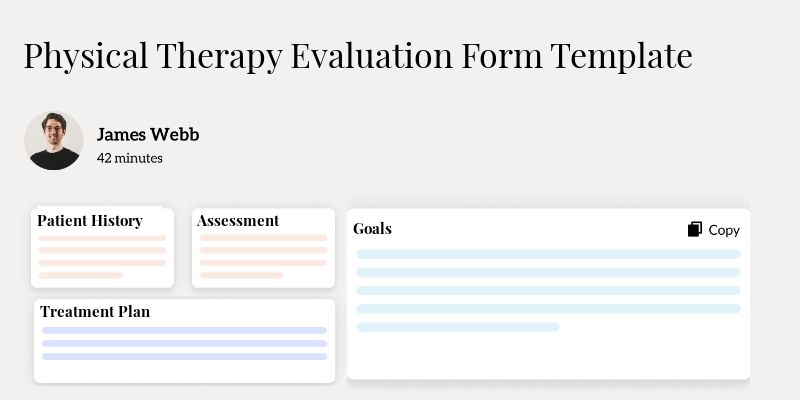
Physical Therapy Evaluation Form Template
Discover practical Physical Therapy Evaluation Form Template templates to enhance your documentation efficiency.

Wellness Wheel Template
Discover practical Wellness Wheel templates to enhance your documentation efficiency.

