
Discharge Summary Template
Key Takeaways
- A discharge summary is essential for a smooth patient transition from hospital to home, encompassing key medical details that improve care continuity and reduce readmission risks.
- Effective discharge summaries include crucial components such as patient information, hospital course, diagnosis, and follow-up care instructions, ensuring clarity and completeness.
- Utilizing standardized templates and tools enhances the quality of discharge summaries, improving communication between healthcare providers and patient understanding of their care plans.
Searching for a discharge summary template to enhance patient care? This article provides a step‑by‑step guide to crafting one that captures all essential information, ensuring seamless patient transitions and improved health outcomes.
Understanding the Discharge Summary
A discharge summary is a crucial document that facilitates a smooth transition for patients leaving the hospital. It encapsulates essential medical details about a patient’s care during their treatment, including the discharge diagnosis. Proper clinical documentation, including discharge notes, significantly impacts the quality of patient care, playing a pivotal role in recovery and continuity.
Without structured discharge summaries, patient care can suffer significantly. Inadequate documentation can lead to confusion, errors in medication administration, and even readmissions.
These summaries offer a comprehensive overview of a patient’s therapeutic journey, covering treatment, progress, and discharge status, ensuring all healthcare providers are aligned. This meticulous documentation enhances patient satisfaction and lowers the risk of readmissions.
Key Components of an Effective Discharge Summary
An effective discharge summary is composed of several key components that ensure clarity and completeness. First and foremost, it must include patient details such as name, date of birth, sex, and medical record number. The summary should clearly state the reason for hospitalization and provide a well‑defined diagnosis, detailing treatments provided and the patient’s condition at discharge. This structured format helps in creating a concise summary that is easy to understand and follow.
Equally important are the follow‑up care instructions. These should include appointments, medications prescribed, and any necessary lifestyle recommendations. The physician’s signature on the discharge summary confirms the accuracy and completeness of the documented information, ensuring that no detail is overlooked.
By adhering to these components, healthcare providers can create effective discharge summaries that facilitate seamless transitions in patient care.
How to Create a Discharge Summary Template
Creating a discharge summary template requires structuring the document to include all necessary information. A structured summary offers a framework that ensures no relevant details are missed.
Mentioning relevant healthcare providers and acknowledging their contributions is essential before finalizing the discharge summary. Tools like TextExpander can streamline the process, allowing quick insertion of commonly used phrases and fields, resulting in thorough and efficient summaries.
Patient Information
The patient information section is the cornerstone of any discharge summary. It must include accurate and comprehensive details such as the patient’s full name, medical record number, and dates of admission and discharge. This information is essential for effective communication among healthcare providers, ensuring that everyone involved in the patient’s care has access to the same vital information.
Detailed information helps maintain continuity of care and facilitates smoother transitions between providers. It ensures the patient’s medical history and current condition are well‑documented, providing a clear picture for subsequent healthcare providers. Such meticulous attention to detail is a vital part of the therapeutic process.
Hospital Course and Procedures
Documenting the hospital course and procedures is critical for a comprehensive discharge summary. This section should detail both surgical and non‑surgical interventions during the patient’s brief hospital course, providing healthcare providers with a thorough understanding of the patient’s hospital experience and care.
This thorough documentation is vital for tracking the patient’s progress and ensuring quality care. It informs future health management and assists in providing a holistic view of the patient’s treatment.
Such detailed records are invaluable for subsequent healthcare providers who will continue the patient’s medical history beyond the hospital walls.
Follow-Up Care Instructions
Follow‑up care instructions are critical in a discharge summary. They should detail follow‑up appointments, prescribed discharge medications, and necessary lifestyle adjustments. Clear and comprehensive discharge instructions prevent confusion and errors in post‑discharge patient care.
These instructions should cover various aspects of the patient’s recovery, including diet, exercise, medication, and signs of potential problems. Additionally, it’s important to highlight any outstanding test results that require follow‑up. Thorough documentation of follow‑up care instructions supports patient recovery and helps prevent complications.
Example of a Discharge Summary Template
Consider an example of a discharge summary template featuring Kevin McAllister, who received recommendations for continued outpatient therapy upon discharge. This template includes patient information, hospital course, discharge diagnoses, and follow‑up care instructions in a structured format, ensuring all necessary details are covered.
Another example features a patient with gastroenteritis who received IV fluids and antibiotics, indicating improvement during the patient’s hospital stay. This template also includes follow‑up care instructions, such as dietary recommendations and medication details, ensuring that the patient understands their care plan after discharge.
A third example involves a patient with asthma who was treated for pneumonia. This discharge summary includes information about medication changes, follow‑up plans, and any necessary lifestyle adjustments. These examples highlight the importance of including all key components and providing detailed information to ensure effective patient care and continuity.
Benefits of Using a Discharge Summary Template
Using a standardized template for discharge summaries offers numerous benefits. It enhances documentation clarity and completeness, making it easier for healthcare providers to follow. These summaries act as critical communication tools, reducing the risk of errors during patient transitions and improving overall care quality.
Additionally, a discharge summary helps patients understand their medical condition, follow‑up care, and medication details. This understanding is crucial for their recovery and compliance with treatment plans. A pre‑formatted discharge summary provides more information due to its structured nature, ensuring that no detail is overlooked.
Tools and Resources for Creating Discharge Summaries
Several tools and resources are available to aid healthcare professionals in creating and managing discharge summaries. pdfFiller, for instance, is a cloud‑based solution that enables users to create, edit, and manage discharge summary documents and forms. This platform offers flexibility and convenience, making it easier to produce accurate and comprehensive discharge summaries.
Another valuable resource is Twofold Health, which provides structured templates to ensure the inclusion of all vital information. This tool helps streamline the clinical documentation process, allowing healthcare professionals to efficiently create discharge notes.
Leveraging these tools allows healthcare providers to enhance the quality and efficiency of their discharge summaries.
Common Mistakes to Avoid When Writing Discharge Summaries
Common mistakes in writing discharge summaries can jeopardize patient care. One significant issue is document legibility, especially with carbon copies. Poor handwriting or unclear print can cause misunderstandings and errors. Additionally, many summaries fail to document investigation results, leaving gaps in patient records.
Another common mistake is the lack of follow‑up advice, with 93% of discharge summaries lacking this critical information. This omission can cause confusion and hinder the patient’s recovery process. Furthermore, 11% of discharge summaries were not signed by doctors, raising concerns about the accuracy and completeness of the documented information.
Resistance to changing current practices also hinders the adoption of structured discharge summaries. Educating physicians and staff about the importance of thorough and accurate documentation can help overcome these deficiencies. Not submitting the discharge summary can result in incomplete patient records. This may create risks for continuity of care and cause billing issues. By avoiding these common mistakes, healthcare providers can create more effective discharge summaries.
Ensuring Continuity of Care with Discharge Summaries
Discharge summaries are crucial for maintaining the continuity and coordination of patient care. Effective communication in discharge summaries ensures a smooth transition for patients to subsequent levels of care. Using a uniform template enhances the accuracy and thoroughness of patient care documentation across various healthcare providers.
A structured template helps reduce the chances of mistakes and missing information, which can adversely affect patient health outcomes. The inclusion of detailed discharge summaries can significantly decrease hospital readmissions by ensuring proper follow‑up care.
By prioritizing the continuity of care, discharge summaries play a vital role in patient recovery and health management.
Discharge Notes with Twofold
Twofold Health simplifies discharge documentation with its customizable templates, ensuring every critical detail is captured efficiently. Whether you need a standard format or tailored sections, Twofold provides the flexibility to streamline your workflow while maintaining accuracy and clarity. Enhance patient care transitions with a discharge note solution designed for precision and ease.
Summary
In summary, discharge summaries are indispensable tools in patient care, ensuring smooth transitions and continuity of care. By understanding the key components and creating structured templates, healthcare providers can enhance the clarity and completeness of these documents. Detailed follow‑up care instructions, accurate documentation of hospital courses, and the use of standardized templates are all crucial for effective discharge summaries.
In conclusion, well‑crafted discharge summaries not only improve patient outcomes but also enhance overall healthcare efficiency. By avoiding common mistakes and utilizing available tools and resources, healthcare providers can create summaries that support patient recovery and reduce the risk of readmissions. Remember, the goal is to ensure that every patient leaves the hospital with a clear and comprehensive plan for their continued care.

Michael Tzach
Michael is a tech leader with expertise in health tech, specializing in innovative software solutions that enhance healthcare efficiency and compliance.
- Prioritize Clarity: Use concise, structured language for seamless understanding.
- Focus on Follow-Up: Highlight essential post-discharge actions.
- Standardize: Utilize templates for consistency and efficiency.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

DAP Note Template
Discover practical DAP Note templates to enhance your documentation efficiency.

Notice of Privacy Practices Template
Discover practical Notice of Privacy Practices Template templates to enhance your documentation efficiency.
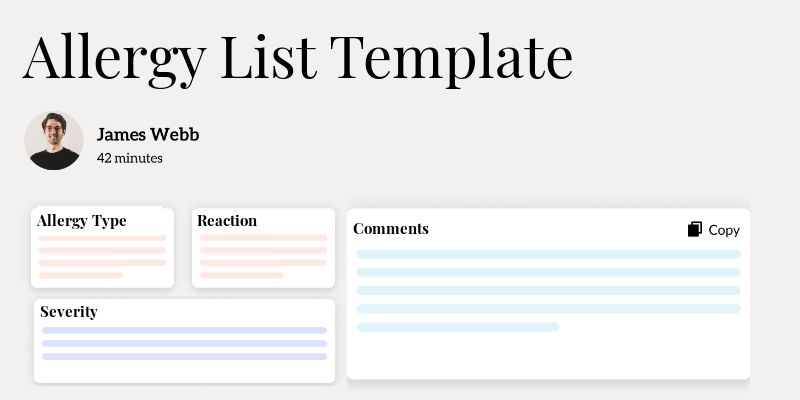
Allergy List Template
Discover practical Allergy List Template templates to enhance your documentation efficiency.


