
Best AI Scribe Tools in 2025: Features, Benefits and Pricing

Envision a workday where your clinical documentation is finished minutes after a patient visit—no more after‑hours charting or rushing to remember key details. This is the promise of an AI scribe: a digital solution that turns live or recorded patient conversations into accurate clinical notes, freeing up time for better patient interaction and letting you leave work at work.
In this article, we’ll explore the best ai scribe tools available in 2025. Whether you’re a small clinic or a large hospital, these tools can transform how you document patient encounters and interact with healthcare providers across the board.
What is an AI scribe?
An AI scribe is a software solution designed to handle repetitive documentation tasks. It listens to your patient conversations, then uses natural language processing (NLP) and machine learning to produce clinical notes in real time or shortly after. By automating transcription and structuring your notes, an ai scribe does much of the heavy lifting in clinical documentation, allowing you to focus on patient care.
Core Functions of an AI Scribe
- Speech-to-Text Transcription: Converts audio from patient encounters into written text.
- Real-Time Note Generation: Processes live discussions and produces clinical notes almost instantly.
- Contextual Understanding: Recognizes medical terminology, patient details, and specialized vocabularies for your specific field.
- Integration with EHRs : Often links up with electronic health record systems, reducing the hassle of copying and pasting patient data.
- Compliance and Security: Typically includes HIPAA-compliant safeguards and end-to-end encryption.
Top 10 AI scribe tools for 2025
The following list outlines ten best AI medical scribe platforms that various clinicians and professionals have found valuable.
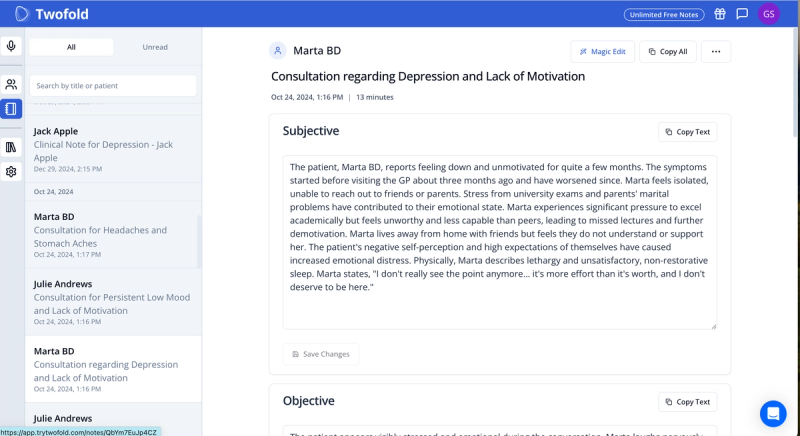
1. Twofold
Twofold is a real‑time AI medical scribe that adapts to each clinician’s style, making documentation faster and more accurate. It integrates with EHR systems and ensures the high level of accuracy, security and customization.
Key Features
- 99% transcription accuracy with minimal need for manual correction
- AI-driven CPT/ICD-10 coding suggestions
- Specialty-based note templates
- Option to create your own templates
- Automated patient progress tracking capabilities
- Multi-language support: 25+ languages including English, French, and Spanish
- HIPAA-compliant with enterprise-grade security
- Built-in analytics and reporting features
Pricing
- Free plan with 20 notes/month.
- $49/month unlimited access and usage.
- Group plans with volume discounts and premium offerings.
2. Nabla
Nabla is an AI medical assistant that transforms clinical interactions into structured notes within seconds. It is widely adopted across specialties and integrates seamlessly with EHR systems.
Key Features
- High transcription accuracy with minimal need for manual correction
- Near-instant note generation
- Specialty-based note templates
- Pre-charting and automated medical coding
- HIPAA, GDPR, and SOC 2 Type 2 compliant
- Real-time clinical decision support
- Multi-language support, including English, French, and Spanish
Pricing
- Free trial available
- Paid plans start at $119 per month

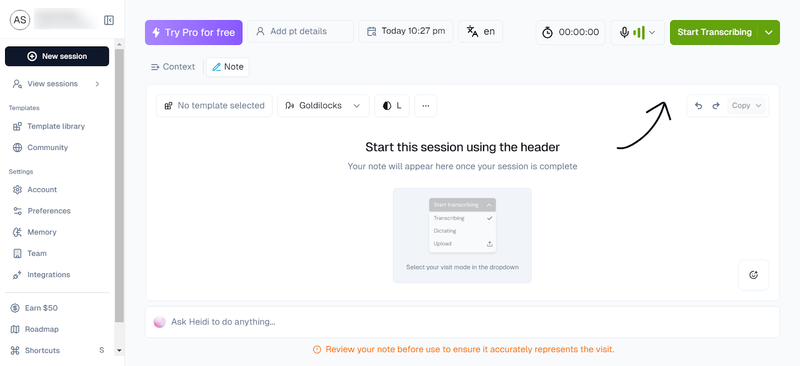
3. Heidi
Heidi is an ambient AI scribe that listens to conversations and generates clinical documentation with minimal user input. It is designed for hands‑free, real‑time transcription and adapts to different specialties.
Key Features
- Real-time documentation with voice-activated commands
- Adaptive learning to match individual clinician styles
- Customizable templates and automated form-filling
- Multi-user collaboration tools
- Supports multiple languages
Pricing
- Free basic plan available
- Paid plans start at $99 per month
4. Athelas Scribe
Athelas Scribe is a real-time transcription tool built to handle multi‑speaker environments, various accents, and background noise. It includes automated medical coding recommendations, making it a good fit for high‑volume practices.
Key Features
- 99.4% transcription accuracy
- Multi-speaker recognition for extended conversations
- Generates SOAP notes, progress notes, and medical forms
- AI-driven CPT/ICD-10 coding suggestions
- HIPAA, SOC2, and HITRUST compliant
- Customizable formatting and templates
Pricing
- Free plan with 10 scribes
- Paid plans start at $149 per month

5. NoteMD
NoteMD provides a record-and-review approach, allowing clinicians to document visits in real‑time or through uploaded audio. It is accessible across multiple devices and offers automatic SOAP note generation.
Key Features
- Works across mobile, tablet, and desktop
- Real-time transcription
- Auto-generates SOAP notes
- Direct EHR integration
- Multi-language support (English, Spanish, French)
- HIPAA-compliant with strict security protocols
Pricing
- Free trial with 10 visits
- Paid plans start at $99 per month

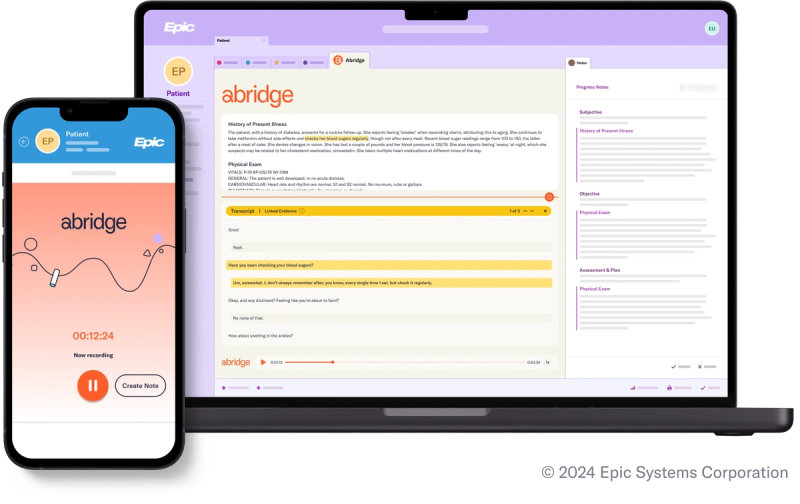
6. Abridge
Abridge is an AI‑powered scribe that automates clinical documentation using generative AI. It extracts key points from clinician‑patient conversations, reducing the need for manual note‑taking.
Key Features
- 91% AI-generated structured notes
- Recognizes medical terminology across 50+ specialties
- Supports over 28 languages
- EHR-integrated workflows, including Epic compatibility
- HIPAA-compliant with enterprise-grade security
- Built-in analytics and reporting features
Pricing
- Custom pricing based on clinic needs
7. Upheal AI
Upheal AI focuses on quick documentation turnaround with an intuitive, easy‑to‑use platform. It is designed for seamless integration into clinical workflows without requiring extensive training.
Key Features
- Minimal setup, easy adoption for clinicians
- Quick transcription and note generation
- Integrates with various EHRs
- HIPAA-compliant security measures
Pricing
- Custom pricing based on practice size and needs

8. Sunoh.ai
Sunoh.ai is a high‑speed AI medical scribe that offers scalable transcription solutions for clinics handling large volumes of patient visits. Its cloud‑based system ensures efficiency and reliability.
Key Features
- Instant transcription processing
- Cloud-native architecture for large-scale operations
- Customizable access permissions for compliance
- High-speed performance in real-time
Pricing
- Usage-based pricing with enterprise licensing available
9. Blueprint AI
Blueprint AI adds predictive analytics to traditional AI scribing, helping clinicians analyze patient data trends while maintaining accurate documentation.
Key Features
- Predictive metrics for risk assessment
- Customizable dashboards
- Large-scale compatibility for multi-site practices
- Direct integration with EHR platforms
Pricing
- Modular pricing with base transcription services and optional analytics add-ons

10. Mentalyc
Mentalyc is specifically designed for mental health professionals, offering detailed documentation support with built‑in emotion and sentiment analysis.
Key Features
- Emotion tracking to highlight important moments in therapy
- Real-time transcription with structured note creation
- HIPAA-compliant security measures
- Session playback with synchronized audio and transcript
Pricing
- Multiple plans based on transcription hours and analytics needs

Best AI Scribe Tools: Feature & Pricing Comparison
AI Scribe | Standout Feature | Pricing |
|---|---|---|
Twofold | Best combination of accuracy, customization and security. | $49/month |
Nabla | Instant structured notes | Starts at $119/mo |
Heidi | Ambient AI with voice commands | Starts at $99/mo |
Athelas | 99.4% accuracy, CPT/ICD-10 automation | Starts at $149/mo |
NoteMD | SOAP note automation, multi-language support | Starts at $99/mo |
Abridge | Generative AI for structured notes | Custom |
Upheal | Quick transcription with minimal setup | Custom |
Sunoh.ai | Cloud-based, high-speed AI transcription | Usage-based |
Blueprint AI | Predictive analytics for risk assessment | Modular |
Mentalyc | Sentiment analysis and therapy tracking | Custom |
Benefits of using AI scribes
- Better Workflows: An AI scribe can drastically cut the time spent on manual note-taking.
- Accurate Transcriptions: With advanced NLP, these tools reduce human error in documenting patient data.
- Increased Face-to-Face Time: When your hands aren’t tied to a keyboard, you can focus on truly listening to the patient.
- Better Work-Life Balance: Finish your documentation during or immediately after a patient visit, so you don’t end up bringing work home.
- Consistency in Notes: Automated transcription ensures standardized clinical notes, improving clarity for follow-ups and referrals.
AI scribes use cases
1. Automating Meeting Summaries
In non‑clinical settings, an AI scribe can capture essential points from staff meetings or multidisciplinary team reviews.
- Real World Example: A large marketing agency hosts daily stand-up meetings with a cross-functional team of creatives, project managers, and account executives. Instead of manually taking notes, they use an AI scribe to transcribe key discussion points in real time. Within minutes of each meeting, the scribe automatically emails a concise summary outlining action items, deadlines, and responsibilities to every participant—ensuring everyone is aligned and accountable for their tasks.
2. Enhancing Medical Documentation
For health professionals, an AI scribe offers a perfect way to reduce manual charting and align seamlessly with electronic health record (EHR) systems.
- Real World Example: A mid-sized primary care clinic recently integrated an AI scribe into their existing EHR. Physicians record patient visits via a simple mobile app, and the scribe transcribes the conversation into structured SOAP notes. Because the notes automatically sync with the EHR, doctors no longer spend hours each evening catching up on documentation. The clinic reports a 25% reduction in charting time and an improvement in overall documentation accuracy, allowing providers to focus more on patient care.
3. Streamlining Legal Transcription
Law firms and compliance officers can also benefit by automating depositions and contract discussions with an AI scribe.
- Real World Example: A busy law firm handling multiple depositions every week introduced an AI scribe to capture and transcribe each session. The AI tool swiftly identifies speaker changes and legal terminology, generating a coherent transcript shortly after the deposition ends. Paralegals can then review the automatically generated notes for accuracy, annotate key points, and share them with the legal team for case preparation. This streamlined approach has slashed transcription turnaround times and significantly reduced administrative costs.
How to choose the right AI scribe tool
- Accuracy Focus: Look for platforms that handle complex medical terms with minimal edits.
- Privacy & Compliance: Confirm robust encryption and HIPAA adherence if handling U.S. patient data.
- Integration: Seek solutions that blend smoothly with your existing software, including your EHR.
- Real-Time vs. Post-Visit: Decide if you need live transcription or if after-the-fact scribing is sufficient.
- User Interface: A simple, intuitive interface often leads to better adoption among busy staff.
- Multilingual Capabilities: If you serve a diverse population, verify it supports multiple languages.
- Scalability: Ensure the tool can keep up if your practice or institution handles large volumes of patient encounters.
The future of AI scribes and emerging trends
- Adaptive Learning: Expect AI scribes to evolve quickly, learning from each user’s corrections and specific medical jargon.
- Stronger Security: As data regulations tighten, solutions may come with more sophisticated encryption and access controls.
- Generative AI Integration
We may see deeper AI-driven analysis, suggesting next steps or offering risk assessments in addition to note-taking.
Conclusion
Choosing the best AI scribe hinges on understanding your practice’s unique workflow, volume, and integration needs. With a wide range of tools—from those focusing on mental health to those emphasizing lightning‑fast note generation—you’re sure to find a solution that aligns with your documentation style.
An AI medical scribe not only eases clinical documentation but can also improve the quality of patient encounters by freeing your attention from the EHR screen. And while plenty of platforms exist, Twofold stands out for its adaptive features and strong emphasis on real-time accuracy—ideal for professionals seeking a robust, customizable solution.
As AI continues to evolve, so will scribe technology. Investing in an AI scribe today means a smoother, more efficient tomorrow—where administrative burdens are minimized and more time is spent focusing on what matters: patient care.
Frequently Asked Questions
ABOUT THE AUTHOR
Dr. Danni Steimberg
Licensed Medical Doctor
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

Best Medical Scribe Software (2025) – According to Real Reddit Reviews
Discover the best medical scribe software in 2025 based on genuine Reddit reviews. Find out why Twofold Health AI Scribe is highly recommended by healthcare providers for accuracy and ease of use.

Best Medical Dictation Software of 2025
Discover the best medical dictation tools of 2025, including key features, benefits, and pricing, to simplify clinical documentation and enhance patient encounters.

How to Write BIRP Notes: Template, Examples & Tips
Learn how to write effective BIRP notes with a template, tips, and examples. Improve documentation, speed, and accuracy in mental health therapy sessions.


