
Writing High Quality Clinic Notes—5 Easy Steps

If you’re part of a busy clinic, medical practice, or mental health team, you already know how important it is to document patient encounters accurately. But let’s be honest—writing clinic notes can sometimes feel like a chore. The good news is that it doesn’t have to be complicated or time‑consuming.
In this guide, we’ll walk through five easy steps for creating high‑quality notes that keep your team organized and your patients safe. Along the way, we’ll share templates, tables, and tips to help you refine your process. Let’s dive in!
Step 1: Stay Aware of Legal and Ethical Responsibilities
Clinic notes aren’t just for your records—they’re also a matter of legal compliance and patient privacy. If you’re in the United States, you’ve likely heard of HIPAA (Health Insurance Portability and Accountability Act), which lays out guidelines for handling patient information.
- Protecting Patient Privacy: Keep records secure and only share them with authorized personnel.
- Avoiding Liability: Inaccurate or incomplete notes can lead to misunderstandings—or worse, legal issues.
- Ethical Standards: Write with respect and stay clear of personal biases.
Pro Tip: Check out the official HHS HIPAA Guidelines or browse Google Scholar on HIPAA Compliance for deeper insights.
Common Mistakes to Avoid
- Missing Details – Forgetting vital information like medications or allergies.
- Incorrect Patient Identifiers – Double-check you’re documenting for the right person.
- Subjective Bias – Your note should focus on clinical facts, not personal opinions.
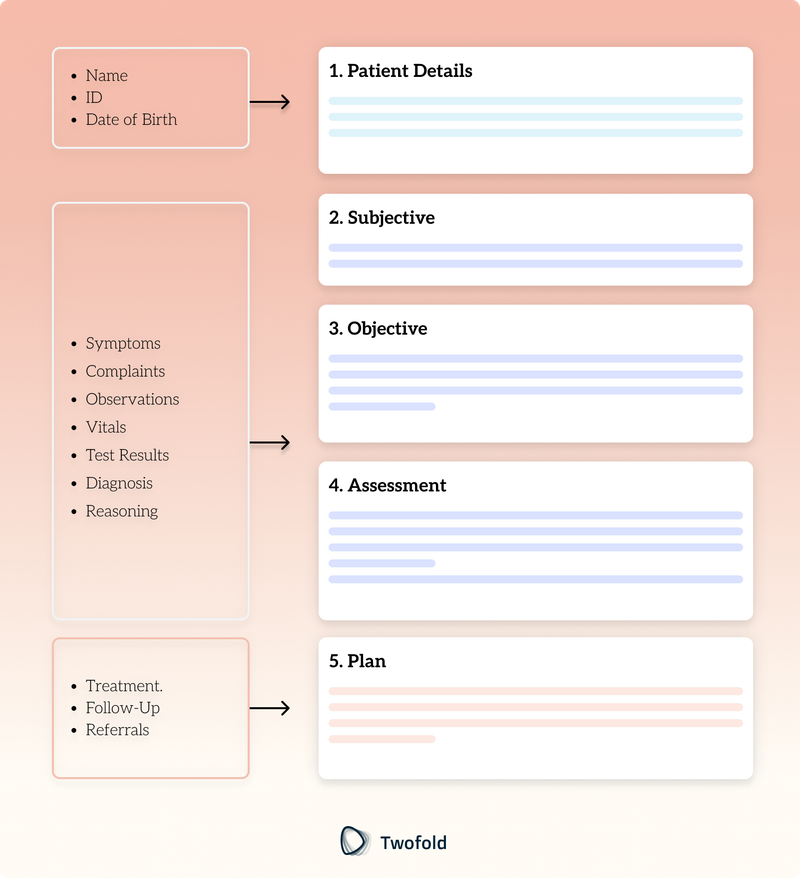
Step 2: Adopt a Standard Structure
If everyone on your team uses a standard layout, it’s easier for anyone—doctors, nurses, mental health therapists—to quickly review and understand what’s happening with a patient. SOAP (Subjective, Objective, Assessment, and Plan) is a common framework.
2.1 SOAP Note Overview
Section | What It Covers | Example |
|---|---|---|
S: Subjective | What the patient reports, including symptoms, concerns, and relevant history. | “Patient reports frequent headaches over the last two weeks.” |
O: Objective | What you or other clinicians can measure—vitals, exam findings, lab results. | “Blood Pressure: 120/80 mmHg, Neuro exam: Normal.” |
A: Assessment | Your clinical impression, including potential diagnoses and reasoning. | “Likely tension headaches; consider stress factors.” |
P: Plan | What comes next—tests, prescriptions, follow-ups, referrals, and patient instructions. | “Prescribe mild analgesics, recommend stress management.” |
Alternative Structures: For mental health, some people use BIRP (Behavior, Intervention, Response, Plan) or DA(R)P (Data, Assessment, Response, Plan). Pick the approach that best fits your setting.
Step 3: Be Clear, Objective, and Concise
3.1 Choose Words Wisely
- Be Direct: Instead of vague terms like “doing better,” use measurable language like “patient reports a 50% decrease in pain.”
- Stay Objective: Avoid adding personal judgments. Stick to facts and observable behaviors.
3.2 Table of Vague vs. Specific Wording
Vague | Specific |
|---|---|
“Patient seems anxious.” | “Patient reported feeling anxious, observed pacing and shaky hands.” |
“Condition is stable.” | “Vital signs unchanged since last visit. BP is 120/75 mmHg, HR is 72 bpm.” |
3.3 Formatting Tips
- Bullet Points for listing vital signs, lab results, or medications.
- Narrative Paragraphs for describing patient stories or complex treatment plans.
Step 4: Use Technology for Accuracy
In the digital age, there’s no shortage of tools that can help you write better, faster, and more accurate clinic notes.
4.1 Electronic Health Records (EHRs)
- Built-In Templates: Many EHRs offer templates that prompt you to fill in key details, so you don’t forget anything important.
- Automated Checks: Some systems can flag inconsistencies or missing data.
4.2 Speech Recognition and Dictation
- If typing is slowing you down, consider speech-to-text tools.
- Make sure to double-check for transcription errors—these tools aren’t perfect yet!
4.3 Clinical Decision Support Systems (CDSS)
- Drug Interaction Alerts: Get a reminder if a patient’s new medication conflicts with existing prescriptions.
- Guideline Suggestions: Some systems highlight standard care paths for specific diagnoses.
Security Note: Confirm that any technology you use meets HIPAA or other applicable privacy standards in your region.
Step 5: Keep Notes Updated and Reviewed
5.1 Regular Audits
- Peer Review: Share a few notes with a colleague and ask for feedback. It’s a great way to catch oversights.
- Self-Assessment: Every few weeks, read over your older notes to see if you’re missing details or using inconsistent formats.
5.2 Ongoing Learning
- Workshops & Webinars: New guidelines and best practices pop up all the time. Stay in the loop by attending training sessions.
- Professional Associations: Organizations like the American Medical Association (AMA) or the American Psychiatric Association (APA) often release updated recommendations.
5.3 Timely Updates
- Immediate Entries: Add or revise info right after patient visits or when you get new test results.
- Version Tracking: If you need to change a note, do it in a way that preserves the history (e.g., adding an addendum).
Quick Reference Table
Step | Key Action | Helpful Tools |
|---|---|---|
| Protect privacy and follow guidelines (e.g., HIPAA). | Official HHS Site, Internal Policies |
| Use SOAP or similar frameworks. | EHR templates, Printed forms |
| Focus on measurable data and observations. | Bullet points, Pain scales |
| Leverage EHRs, dictation, decision support. | HIPAA-compliant platforms |
| Conduct audits, stay up-to-date with new policies. | Peer reviews, Training sessions |
Conclusion
Writing high‑quality clinic notes doesn’t have to be stressful. By following these five steps—staying aware of legal responsibilities, using a clear structure, keeping language concise, using the right tech tools, and regularly reviewing your process—you’ll create notes that are easy to read and meet professional standards.
Remember, the goal is to support better patient care and teamwork. Clear documentation can make all the difference in ensuring patients get the right treatment at the right time. Start small: pick one area to improve, like adopting a SOAP template or trying out a new EHR feature. Over time, these little changes can lead to big improvements for your clinic.
Frequently Asked Questions
ABOUT THE AUTHOR
Dr. Eli Neimark
Licensed Medical Doctor
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

How to Write SOAP Notes: Examples & Template
Learn how to write effective SOAP notes with examples, templates, and best practices. Improve documentation with our detailed guide.

How to Write BIRP Notes: Template, Examples & Tips
Learn how to write effective BIRP notes with a template, tips, and examples. Improve documentation, speed, and accuracy in mental health therapy sessions.

How to Write GIRP Notes: Examples & Template
Learn how to write effective GIRP notes with examples, templates, benefits, and AI tools. Avoid common mistakes and streamline documentation effortlessly.


